States and territories will need additional resources, funding and support to carry-out the most expansive vaccination plan in history.
Summary
NGA surveyed states and territories in November and December on the support, resources and funding needs in order to carry out an equitable and effective COVID-19 vaccination plan. These initial estimates and needs are subject to change, as states and territories are responsible for carrying out the most complex vaccination plan in history. There are still many unknowns as states and territories grapple with assessing the additional support, resources and funding they will need to carry out a plan to inoculate more than 328 million people nationwide. In reviewing the total budgets submitted, many states did not include additional funding for PPE and other equipment and refrigeration needs, however, all responded that this will be necessary in carrying out a vaccination plan. The majority of states and territories have mentioned the need to utilize their National Guard but the additional cost is unknown, therefore this expense was not included in the total budget.
Twenty-seven responses were received to date from states and territories and 21 provided budget projections that lead to a preliminary total budget of $2,144,540,154 to carry out a successful vaccination plan.
Workforce/Staffing Needs
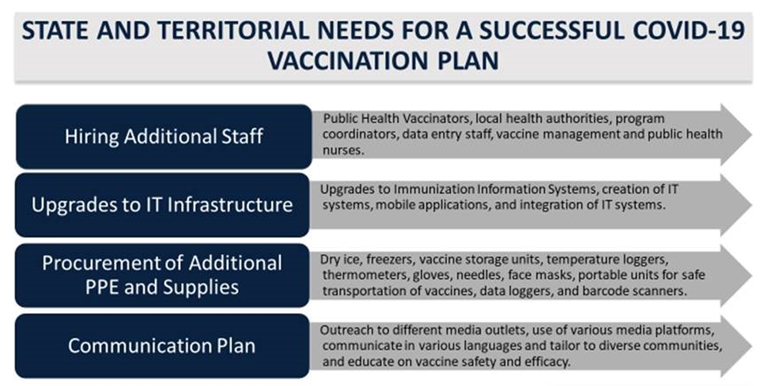
Twenty-seven states and territories specifically mentioned that they will need additional workforce and staff such as public health vaccinators, local health authorities, program coordinators, data entry staff, vaccine management and public health nurses. In addition, states mentioned that they will need PREP Act accommodations, additional administrative staff to fulfill Emergency Use Authorization (EUA) and reporting requirements and for provider enrollment. Additionally, with the increased number of COVID-19 cases and hospitalizations, many states are struggling with finding sufficient staff. Nineteen states and territories responded with a specific budget for hiring additional staff and workforce needs at: $273,400,125.
IT Infrastructure
Nineteen states and territories specifically mentioned that they will need support in upgrading their immunization information systems. This includes: creation of IT systems and associated training and call centers, ongoing enhancements (expansion of current immunization information systems to include additional data fields and mobile applications for off-site vaccinations), and integration of IT systems. Additionally, states have asked for more clarity on privacy, security, and the use of personally identifiable data.
There were questions regarding the federal process to ensure that state and territorial systems are fully capable of executing all processes that will be necessary throughout the vaccination campaign. In addition to funding, one state specifically mentioned having challenges with IT systems, specifically Tiberius. At the time of the survey, Tiberius could not create a vaccine allocation plan that accommodates more than one vaccine. Each vaccine must have its own plan, but sites will be receiving multiple vaccines. This makes that application much more cumbersome than it should be. Seventeen states and territories responded with a total IT infrastructure budget of $68,672,996.
PPE/Refrigeration/Equipment
All respondents noted that PPE and refrigeration were necessary for vaccine distribution and nine are facing PPE shortages at this time. Some states and territories mentioned a shortage of gloves and potential supply chain issues. Per the CDC Playbook, only six face guards (four masks and two face shields) will be provided per every 100-dose shipment of COVID-19 vaccine. There are concerns that needles and syringes also are in short supply, which may be due to competition among local, state and federal agencies purchasing supplies, in addition to private partners, such as hospitals, long-term care facilities and other health care providers. Nine states and territories reported their specific budget to purchase additional PPE/refrigeration/equipment at $243,319,369. The additional equipment and supplies that state and territories indicated they will need to purchase are:
- • Dry ice
- • Freezers
- • Additional vaccine storage units
- • Temperature loggers/thermometers
- • Gloves (and gloves for handling of dry ice) and needles. While gloves for providers to vaccinate are not required, many providers prefer to use gloves and some may be required to wear gloves.
- • Face masks/N95
- • Portable units to support safe redistribution
- • Data loggers
- • Barcode scanners
Vaccine Coverage
Most of the states and territories that responded to the survey are relying on the information that has been provided to them from the Administration that vaccine administration fees will be fully covered for those who are insured, underinsured and/or covered by Medicaid or Medicare. For those who are uninsured, the provider who administers the vaccine will have to submit a claim through the HRSA portal.
There was a concern raised regarding individuals who only have coverage through limited benefit packages for Medicaid, and whether they will be covered. Concerns regarding sufficient funding in the Provider Relief Fund were also mentioned, so having up-front funding to cover administrative costs for the uninsured and underinsured was suggested. In addition, there are concerns regarding the level of reimbursement for COVID vaccine. For the first dose, it is only $16. States and territories are working with Medicaid and insurance companies to cover the administration fee.
One jurisdiction mentioned $13.5 million in costs associated with vaccine administration that will not be reimbursed for those at open and closed pods, including hiring EMS and other contractors to supplement vaccine administration capacity.
Overall states and territories are cautiously optimistic that vaccine doses purchased by the U.S. government will be provided to Americans at no cost and that providers who administer the vaccine will be paid through insurance reimbursement under Medicare and Medicaid, or private coverage. A few noted administration costs that will be incurred by local health departments, and currently are not covered. One important note: The enhanced federal funding and COVID-19 vaccine coverage requirements are tied to states’ receipt of enhanced federal matching funds during the COVID-19 Public Health Emergency (PHE) declaration and only last through the end of the quarter in which the PHE ends. This means requirements to cover a coronavirus vaccine at no cost to enrollees will expire if the PHE is not renewed.
National Guard
To date, 52 Governors – based on the NGA survey and on known letters to the President – have indicated the need for Title 32 authorization for the National Guard for COVID-19 vaccine related activities. This mission was extended Dec. 3 through March 31, 2021, though there are funding ramifications due to a 25 percent cost share requirement. These activities range from logistical support at sites to distribution and handling of the vaccine itself.
Communication and Public Education Campaign
Fifteen states and territories responded that the cost of running a successful public health education campaign will be an additional expense. Concerns regarding the safety and efficacy of vaccines has been and will continue to be a huge hurdle for states and territories to overcome. One state mentioned that it is working on getting vaccination record cards translated into several different languages (CDC only provides them in English and Spanish) and will need to have the EUA patient information form translated quickly.
In addition, in order to ensure the equitable distribution of a vaccine, states and territories must have an effective plan in place for outreach to communities of color, individuals who are vaccine hesitant, and others in their states and territories. To carry out a successful vaccine communications plan, 15 states projected a total cost of $84,810,000.