Governors play a crucial role in shaping policies that can effectively address congenital syphilis rates, promoting the health and well-being of mothers and infants across the United States.
(Download)
Congenital syphilis poses a significant public health challenge in the United States, affecting maternal and child populations. This issue brief provides an overview of what congenital syphilis is, its impact on mothers and infants, and the importance of early screening and treatment. Additionally, it discusses policy considerations for Governors to address the rising incidence and highlights the public health implications of neglecting the surge of congenital syphilis.
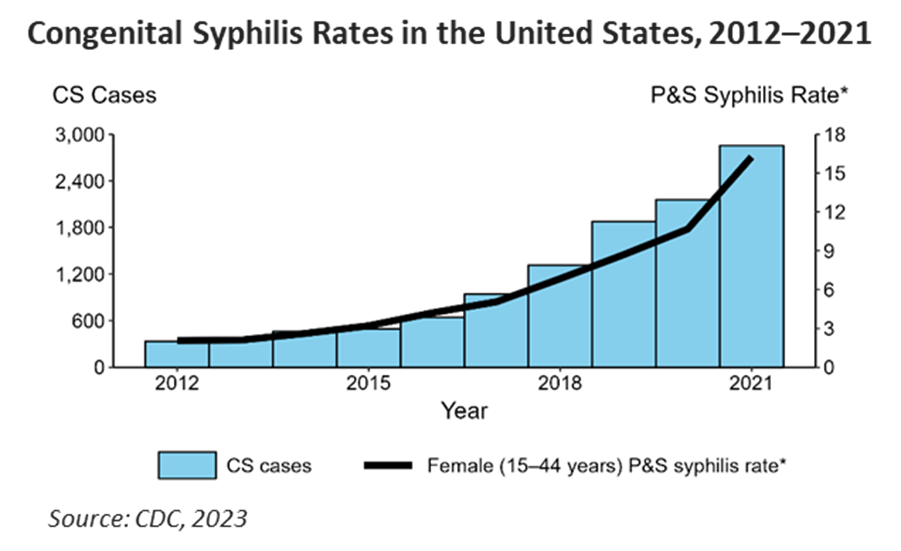
Between 2015 and 2019, there was a nearly 30 percent increase in syphilis cases across the U.S. Specifically, congenital syphilis rates escalated by 582 percent over the last decade. Congenital syphilis rose most among Medicaid beneficiaries, who experience rates six times higher than patients with private insurance. Between 2020 and 2021, 37 states saw rates continue to rise, resulting in 2,855 reported cases. Of those cases, 220 resulted in stillbirth and infant death.
Infants diagnosed with congenital syphilis may experience a range of health issues, including developmental delays, organ damage, anemia and nervous system complications. If left untreated, congenital syphilis can result in long-term health complications, such as blindness and deafness. In addition to major health impacts, congenital syphilis hospitalizations cost an average of $58,000. Furthermore, congenital syphilis disproportionately affects historically marginalized communities. Addressing this issue is essential for achieving health equity and reducing health disparities among different populations.
Congenital syphilis is preventable with timely and appropriate prenatal care, which requires prenatal disease screening and access to treatment. A study evaluating over 100 congenital syphilis cases diagnosed between 2014 and 2018 found that delayed or limited access to prenatal care increased congenital syphilis rates. In many cases, screening for syphilis is not prioritized or available due to a lack of funding or available clinics. For example, states may not have the available funding to bolster their disease intervention specialist workforce whose focus is contact tracing diseases like syphilis that are often dormant for years. This funding often comes from federal grants or must be earmarked in state budgets.
In addition to access issues, low health literacy rates and social drivers such as poverty, stigma around substance use during pregnancy, citizenship status and lack of health care coverage have all been cited as barriers to syphilis testing and treatment. The Centers for Disease Control and Prevention (CDC) refers to health literacy as the ability for individuals “to find, understand, and use information and services to inform health-related decisions and actions for themselves and others.” At least 36 percent of U.S. adults are considered to have low health literacy, which is directly linked to greater health care costs. The U.S. Office of Disease Prevention and Health Promotion has developed a National Action Plan to Improve Health Literacy that sites programs and policy opportunities to improve health outcomes by bolstering health literacy, including community engagement in program design and tailoring communication campaigns to target populations.
Early and universal screening during pregnancy is an effective way to prevent syphilis before it is passed in utero. A 2019 study showed mothers with a syphilis diagnosis over 36 weeks pregnant were 25 times more likely to deliver a baby with congenital syphilis than those diagnosed at 12 weeks or less into their pregnancy.
Congenital syphilis is syndemic with substance use, incarceration and social drivers impacting rising disease rates and related outbreaks. A 2023 CDC Morbidity and Mortality Weekly Report found that mothers delivering babies with congenital syphilis were twice as likely to have used substances (tobacco, alcohol, cannabis or illicit opioids) during pregnancy.
Syndemic: Synergistic epidemics or “the presence of two or more disease states that adversely interact with each other, negatively affecting the mutual course of each disease trajectory, enhancing vulnerability, and made more deleterious by experienced inequities.” Source: The Lancet, 2017

Nearly 40 percent of pregnant women who use substances did not receive prenatal care. A fear of punishment, removal of the infant, imprisonment or other penalties may reduce the likelihood of a pregnant person seek treatment. In 25 states, substance use during pregnancy is considered child abuse and can be grounds for terminating parental rights. To prevent adverse outcomes and future congenital syphilis cases, the Louisiana STD/HIV/Hepatitis Program developed an initiative that empowers clients to make informed decisions about their care and connects women of childbearing age with a syphilis diagnosis to a case manager. The case manager links these women to resource needs, such as food, housing and transportation, as well as health needs, including substance use and mental health care.
Furthermore, people entering correctional facilities have a higher prevalence of syphilis than the general population. Screening and early treatment in jails and prisons can reduce the congenital syphilis rates. For example, the North Dakota Department of Health instituted a rapid syphilis screening program in partnership with county corrections to manage transmission among women in a local jail and provide proper treatment.
The long-term health consequences of congenital syphilis can lead to increased health care costs, special education needs and decreased quality of life for affected individuals. Preventing congenital syphilis is a cost-effective investment in the overall health of society. Additionally, Medicaid beneficiaries are less likely to seek prenatal care than those with private insurance. A study of Medicaid claims data from three states shows average screening rates of 74 percent among women without a recent history of STIs and 84.5 percent for those with a recent history of STIs. For many, Medicaid eligibility is tied to pregnancy, and the change in insurance coverage may result in interrupted care and delayed access to services. Bundled payments, although important in improving the value of care for patients, can also make it difficult to measure screening rates. When providers are reimbursed for a full pregnancy, they may be less likely to report each service, resulting in under reporting of syphilis screening. Depending on coverage and the state’s Medicaid program, those getting tested may need to pay out-of-pocket for the test and get reimbursed, which may pose a barrier to care.
Currently, 42 states require syphilis screening during certain stages of pregnancy, e.g., first trimester through delivery. The United States Preventive Services Task Force (USPSTF) recommends universal screening for all pregnant women, and the CDC recommends screening at the first prenatal visit. For those at high risk for syphilis, previously untested or living in areas of high syphilis morbidity, the CDC also recommends another screening during the third trimester and at delivery.
As of 2021, 16 states required syphilis screening in the third trimester or at delivery. Other states require third trimester or delivery screening only if the patient is determined to have a higher risk. Recently, the Mississippi Board of Health and Department of Health issued an emergency order to adapt screening laws, requiring physicians to test all pregnant people for syphilis at delivery while also stating that providers should ensure appropriate treatment for both syphilis infections during pregnancy and for congenital syphilis infections.
A survey of clinicians and medical students conducted from 2016 to 2017 shows that provider knowledge and awareness of syphilis was low. Another survey from both the CDC and the American College of Obstetricians and Gynecologists found that clinicians also have low awareness of guidelines on syphilis management in pregnancy . Low awareness among clinicians has been attributed to an inadequate public health infrastructure to share knowledge and training among prenatal care providers as well as provide resources for screening and treatment. Providers also cited limited resources to help manage a syphilis diagnosis alongside social comorbidities, e.g., homelessness, poverty and more. Many states, including New York and North Carolina, are spreading awareness to the provider community by issuing health advisories about rising syphilis rates among pregnant women. California hosts in-person provider trainings and encourages providers to complete the National STD Curriculum or virtual syphilis training available from the California Prevention Training Center.
Other states, like Alaska, have dedicated state funding to eliminate congenital syphilis. Alaska Governor Mike Dunleavy’s FY2024 budget devoted $9.5 million to the state’s Department of Health for the healthy families initiative, which includes plans to eliminate congenital syphilis. New Mexico Governor Michelle Lujan Grisham signed a bill during the 2023 legislative session to eliminate copays for STI screening. Some states and health plans are taking it a step further by providing financial incentives for prenatal visits. In 2019, the Oregon Health Authority launched an HIV and syphilis care incentive program that provides gift cards for each treatment visit to pregnant women with syphilis. Similarly, Molina Healthcare, a Medicaid managed care organization, incentivizes prenatal care and healthy pregnancies in Ohio through Molina Rewards 4 Health, rewarding members up to $250 for visiting their doctors and providing free rides to appointments. Similarly, CareSource’s Babies First Program in Georgia allows expecting mothers to receive up to $265 for seeing their doctor regularly.
Congenital syphilis is a preventable and treatable public health issue that requires concerted efforts at the policy and community levels. Governors play a crucial role in shaping policies that can effectively address congenital syphilis rates, promoting the health and well-being of mothers and infants across the United States. Investing in prevention, education and access to healthcare services is vital for achieving positive health outcomes and reducing the burden of congenital syphilis on society.
Authored by Michelle LeBlanc with contributions from Eden Moore












