This publication explores strategies Governors used in their COVID-19 response and ideas for improving future efforts and continued recovery plans.
(Download)
This is the first in a series of five publications focused on COVID-19’s impact on maternal and child health (MCH) programs and populations in the U.S. Each publication focuses on a facet of MCH, including COVID-19 response and recovery, health and human services workforce, childcare, behavioral health, and community supports. The information contained in this series comes from a culmination of interviews and research conducted between early 2022 and January 2024, including an expert roundtable held in the summer of 2022.
Maternal mortality rates are higher in the United States than in similar economically developed countries. Maternal mortality and pregnancy-related death are key indicators of population health and quality of health care delivery. When mothers and parents are absent, families and communities suffer economically and psychologically.
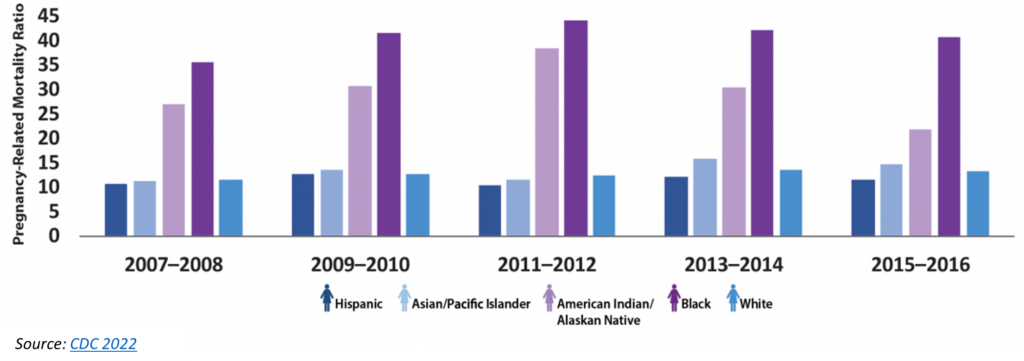
Pregnancy-related deaths in America are preventable in 80 percent of cases. Black and American Indian/Alaska Native (AIAN) women are most impacted and are more likely to die from pregnancy-related causes than White women. This gap, illustrated in Figure 1, has remained consistent, and in 2021, maternal mortality rates for Black women (69.9 deaths per 100,000 live births) were 2.6 times higher than those of White women (26.6 deaths per 100,000 live births). Although an important factor in measuring health, pregnancy-related death is not the only maternal health outcome with an opportunity for improvement across the U.S. Each year, thousands of women experience severe complications resulting from pregnancy and childbirth, known as severe maternal morbidity. In 2019, the impacts of maternal morbidity were estimated to cost the United States around $32 billion, with 75 percent of those costs allocated to long-term health impacts. Additionally, infant mortality, or the death of a child within the first year of life, is higher in the U.S. than in many comparable countries. In 2020, infant mortality rates were highest among Black infants (10.38 per 1,000 live births) compared with all other racial/ethnic groups. Poor birth outcomes in the U.S. are a result of limited access to care, racial and ethnic discrimination, inadequate standardization of care, and other underlying factors. The 2022 March of Dimes Report noted that approximately 2.2 million women of childbearing age lived in counties with no hospitals or birth centers offering obstetric care and no obstetric providers, thus limiting access to appropriate preventive, prenatal and postpartum care. These statistics show a health system struggling with massive inequities – even before a global pandemic exacerbated every aspect of health care, social services, private industry and individual resilience.
The COVID-19 pandemic caused unique disruptions to health and social care programs serving MCH populations. Between school and child care closures, telehealth limitations in maternal care, and preexisting inequities, the pandemic pushed an already Unwieldy system to its limits. Closures and limitations coupled with anxiety, extreme stress, and burnout exacerbated social drivers of health linked to poor health outcomes, especially related to maternity care, mental health, and racial and ethnic disparities. For example, the U.S. maternal mortality rate increased from 20.1 deaths per 100,000 live births in 2019 to 32.9 deaths per 1,000 in 2021. These rates increased across racial and ethnic groups, with the highest rates observed for Black women.
The pandemic upended decades-old health delivery and data systems, caused governments to pass legislation quickly, and required Governors to sign executive orders, especially in the first phase of COVID-19. Transitioning to endemic COVID-19 has been slower, allowing policymakers to consider deliberate actions and strategies to improve public health infrastructure for the MCH population and beyond.
MATERNAL HEALTH TERMINOLOGY
Maternal death: Death of a pregnant or birthing person during pregnancy or up to 42 days after the end of pregnancy from pregnancy-related complications.
Pregnancy-related death: Death of pregnant or birthing person during pregnancy or within one year of the end of pregnancy from any cause related to or aggravated by the pregnancy
Governors’ Strategies
This publication explores strategies Governors used in their COVID-19 response and ideas for improving future efforts and continued recovery plans. Some of these efforts include:
- Convening advisors, community members, agency leaders, public/private organizations, elected officials, beneficiaries and others to provide diverse perspectives on policy implications.
- Improving data collection and monitoring, especially related to self-reported data points like race, housing status and gender.
- Exploring options to extend postpartum Medicaid coverage to 12 months.
- Identifying COVID-era legislation to continue guidance increasing access to health care, including telehealth.
Convening Varied Groups to Provide Diverse Policy Perspectives
The COVID-19 pandemic disproportionately impacted certain communities and individuals in various ways, whether directly with infection or more nuanced circumstances. For example, Black, Hispanic and AIAN communities saw higher case and death tolls and less access to mitigation measures than White counterparts. The stress of the pandemic mixed with stay-at-home orders correlated to an eight percent increase in intimate partner violence. The lockdown also limited options for survivors to access help, that is, if services continued operating. Understanding specific challenges individuals experienced due to COVID-19 can inform policies, providing carveouts for those disproportionately impacted to rectify current hardships and better plan for future disasters. To do this, Governors and state leaders can create opportunities to involve people with varied perspectives and lived experiences. Not only does this engender trust between the government and residents, but it also allows policymakers to address barriers and gaps.
STATE ACTIONS
Vermont Governor Phil Scott partnered with the Office of Racial Equity in his COVID-19 command structure. Decision-making and planning were informed by the Office, especially elements related to the state’s immigrant and refugee communities. The Office partnered with the Association for Africans Living in Vermont to create linguistically appropriate COVID-19 guidance for this community. The Office, in conjunction with the State Performance Officer and the Governor’s Office, also created an equity impact assessment to ensure budgetary and programmatic proposals align with state equity goals.
Due to social, geographic, political, economic and environmental factors, COVID-19 mitigation efforts (testing and vaccination) were also less accessible to specific groups. The Minnesota Department of Health’s COVID-19 vaccination data showed a gap in uptake among African American, East African, American Indian and Latina women of childbearing age. The Department held listening sessions to understand specific concerns within these communities, allocated necessary resources and created a network of trusted messengers to build confidence in their government. Distrust in the vaccine and/or government was part of the apprehension for some of the women in these communities. Although COVID-19 vaccine confidence has been an issue, access to vaccination clinics and providers also affected uptake. Vaccinator access is especially important for children who fell behind on routine childhood immunizations during the pandemic – an issue that impacted nearly 27 percent of U.S. households surveyed in 2021. To improve access, especially in rural areas with limited providers, the Vaccines for Children programs in New York and Utah enrolled independent pharmacists to administer vaccines and increase access for children in low-income or uninsured households.
In addition to the examples outlined above, Governors may also consider:
- Creating a task force of multidisciplinary experts to address the effect of COVID-19 on pregnant women and new mothers.
- Examining potential policy actions that will provide pregnant women and new mothers with alternatives to hospitalization, such as birth centers or home births.
- Encouraging state agencies to work with providers to create outpatient assessment tools that help monitor mother and baby.
- Leveraging state maternal mortality review committees and perinatal quality collaboratives in policymaking with implications for MCH populations, e.g., pregnant individuals, parents, caregivers, children, babies, adolescents, women, families, etc.
- Collaborating with state immunization managers, MCH directors and other relevant agencies to strategize on increasing routine childhood immunizations to pre-COVID levels.
- Issuing a Governor’s Proclamation to recognize August as National Immunization Awareness Month to increase awareness of routine immunizations and provide families with additional opportunities to receive routine vaccines.
- Supporting vaccine awareness by leading routine immunization campaigns and partnering with trusted, local community leaders to increase awareness of the importance of immunizations and information on where/how/when to get them.
- Expanding vaccinator eligibility to pharmacists for certain age groups.
- Encouraging partnerships between public health, public safety, emergency management and MCH leads to develop and maintain emergency plans with specific logistics for the MCH population and codifying these plans for future crises.
- Developing plans to monitor pregnant and postpartum people, parents, babies, and children in unsafe environments such as those experiencing homelessness or living in a domestic violence situation during disease outbreaks, extreme weather, and other public emergencies and refer them to appropriate, safe services.
STATE ACTIONS
To better respond to the pandemic, the Oregon Health Authority’s Public Health Division provided funding and resources to 173 community-based organizations. Organizations applied for grants to foster community engagement, education and outreach; conduct contact tracing; and, provide social services and wraparound supports. The program allowed the state government to improve access to community-driven, culturally and linguistically appropriate public health services while building strong, responsive relationships with the community.
Improving Data and Surveillance
Minnesota’s example above illustrates how data can be used to reduce disparities and address new or ongoing challenges. COVID-19 contact tracing, testing, and vaccination data were at the forefront in 2020 and 2021. State health leaders were inundated with interoperability issues within their data systems, across state lines, and with federal systems. This was especially true when state health departments needed to connect COVID-19 cases or vaccine data with pregnancy and newborn data. Many states created new opportunities to connect the dots on data. For example, Ohio used funding from the American Rescue Plan Act (ARPA) to increase interoperability to identify the number of COVID-19 cases among pregnant and postpartum women and measure that alongside their vaccination status to determine uptake.
Many state data systems were outdated prior to the pandemic, and COVID-19 pushed them beyond their capacity. Most systems did not collect appropriate data, including self-reported points like race, ethnicity, gender, etc. Utah Governor Spencer Cox authorized ARPA funding for data modernization to both increase interoperability between the state’s health and corrections departments and determine better ways to collect data on race and ethnicity. In Oregon, the state’s health data infrastructure already collected data by race, ethnicity, language and disability, allowing them to address actual needs as trends emerged.
In addition to the examples outlined above, Governors may also consider:
- Encouraging payers, providers, health systems and other stakeholders to collect data on race, ethnicity, disabilities, gender identity, geographic location and other self-reported data points to establish inclusive data sets that illustrate the health of specific groups and capture intersectional challenges.
- Allocating funding to modernize public health data systems.
STATE ACTIONS
New Jersey Governor Phil Murphy signed legislation in May 2019 formalizing the Maternal Data Center. Having this in place allowed the state to collect and analyze data on MCH populations more nimbly. Furthering the state’s data modernization efforts, Governor Murphy signed additional legislation in January 2020 creating regional health hubs. The four hubs are placed in strategic regions of the state and foster collaboration and data sharing across local organizations. Each hub operates a Health Information Platform to understand the needs of each region.
Extending Postpartum Medicaid Coverage
With the passage of the ARPA, Governors are now able to direct their Medicaid programs to submit a state plan amendment (SPA) to extend coverage to postpartum women for 12 months. Prior to this provision, state Medicaid programs had to submit a request for a waiver of federal rules under Section 1115 of the Social Security Act to extend postpartum coverage. The waiver process is more cumbersome than an SPA and must be renewed every five years. Four in ten births in the U.S. are covered by Medicaid – making it one of the largest payers for birth in the U.S. Extending Medicaid coverage for postpartum women may prevent as many as 45 percent of women from being disenrolled after the required 60-day coverage period ends. States opting to extend coverage aim to close coverage gaps, improve maternal and infant health outcomes and reduce maternal mortality, which rose during the first year of the pandemic. Since this provision went into effect, 38 states, the District of Columbia, and the Virgin Islands have implemented a 12-month extension, and ten states are planning to do the same.
In addition to the examples outlined above, Governors may also consider:
- Determining legislative, budget or agency barriers that would prohibit postpartum Medicaid extension and collaborate with the appropriate groups to overcome barriers.
- Collaborating with the state Medicaid agency to create a proposal to the Centers for Medicare and Medicaid Services to extend postpartum Medicaid coverage to 12 months through an 1115 waiver or State Plan Amendment.
- Holding discussions with the legislature to address any concerns and provide education on the benefits postpartum Medicaid extension would have for the state.
Codifying COVID-Era Guidance with Demonstrated Support and Benefit
The swift start of the pandemic required Governors to act immediately to “flatten the curve” or prevent a spike in new COVID-19 infections. Governors and state health officials released sweeping policy changes to address immediate pandemic concerns, including stay-at-home orders, options for virtual services and allowances for providers to practice across state lines. As the pandemic dragged on, Governors and state health officials enacted temporary flexibilities for frontline workers addressing direct impacts of the pandemic, including in telehealth, scope of practice and state licensure. As state public health emergencies around COVID-19 end, some states are codifying those temporary policy changes and developing long-term policies. For example, many states required insurance payers to reimburse providers the same amount for telehealth and in-person services during their public health emergencies. As many of these emergencies have ended, 21 states have codified payment parity requirements; eight other states implemented parity with caveats on the period or reimbursable services. For example, the Minnesota Department of Human Services allowed providers to continue practicing virtually as appropriate. Some of those providers work in intensive treatment in foster care and children’s residential facilities or serve as doulas, community health workers, alcohol and drug counselors and mental health workers in a variety of capacities.
In addition to the examples outlined above, Governors may also consider:
- Supporting legislation that continues executive orders or other COVID-era guidance allowing appropriate social and health services to be provided virtually and reimbursed.
- Incorporating child welfare options in telehealth policies to increase access to specialized medical and mental health expertise, enhance staff capacity, reduce time barriers and provide options for clients who may prefer remote options.
- Codifying legislation to allow providers to practice across state lines where appropriate.
Conclusion
The pandemic pushed state government systems to their limit, highlighting various issues and requiring Governors and state health officials to act quickly. State governments, led by their Governors, are now tasked with developing long-term plans and preparations for future emergencies. COVID-19 illustrated the importance of strong public health infrastructures, which only comes with an eye toward equitable access and input from the populations that will be impacted the most.
Acknowledgments
The NGA Center would like to thank the state officials and experts who participated in the June 2022 expert roundtable as well as those who provided feedback to inform this publication. The NGA Center would also like to thank the Health Resources and Services Administration in the U.S. Department of Health and Human Services for their generous support of this project. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of HRSA or the U.S. Department of Health and Human Services.
This publication was developed by Michelle LeBlanc, Asia Riviere, and Brittney Roy at the National Governors Association Center for Best Practices.
Recommended citation: LeBlanc, M., Riviere, A., & Roy, B. (2024). State Strategies to Address the Impact of COVID-19 on Maternal and Child Populations: COVID-19 Response and Recovery. Washington, D.C.: National Governors Association Center for Best Practices.