This papers pulls together considerations and examples of best and promising practices for Governors, including building vaccine confidence through consistent, transparent and factual communication; establishing straightforward pathways for individuals to access vaccines; and, developing and streamlining sustainable systems to strategically allocate and distribute vaccines to rural and frontier populations.
(Download)
Access to health care is a common challenge for rural and frontier communities due to provider shortages, insufficient broadband Internet availability, geographic location and other issues. The COVID-19 pandemic has exacerbated many of these barriers. Rural residents often travel longer distances to receive the COVID-19 vaccine than people in other areas, and they generally lack access to public transportation. Rural residents may also struggle to receive critical public health information due to unreliable access to the Internet and other technology equipment, such as smartphones and computers. During the pandemic, additional challenges surfaced including a lack of trust in the government and concern about the COVID-19 vaccine’s safety. The fast-paced nature of the pandemic spurred new and changing information with misinformation spreading as quickly as reliable news, undercutting science and public policies, especially related to COVID-19 prevention measures like the vaccine.
Governors have the authority to pull together stakeholders and the ability to address the long-standing and emerging issues impeding vaccine confidence, access and uptake in rural communities. Because trusted messengers are vital to increasing confidence, Governors might consider convening state experts and local partners to establish a strong foundation of trust. They may also allocate resources to build on existing programs and processes and create new, sustainable strategies that will both improve vaccination rates as the pandemic continues and prepare future public health initiatives.
Considerations for Governors
The National Governors Association Center for Best Practices (NGA Center) conducted interviews with state officials, national experts and rural community-based organizations to determine best and promising practices Governors can use to promote vaccine uptake and confidence in rural communities. These strategies were further vetted by experts during a roundtable in June 2021. The research and roundtable discussion culminated in the strategies and examples within this report. The strategies fell into the following thematic areas:
- Building vaccine confidence among rural communities through consistent, transparent and factual communication strategies and campaigns.
- Establishing straightforward pathways for individuals in rural areas to access vaccines within their communities.
- Developing and streamlining sustainable systems to strategically allocate and distribute vaccines to rural and frontier populations.
Consideration 1: Build vaccine confidence among rural communities through consistent, transparent and factual communication strategies and campaigns.
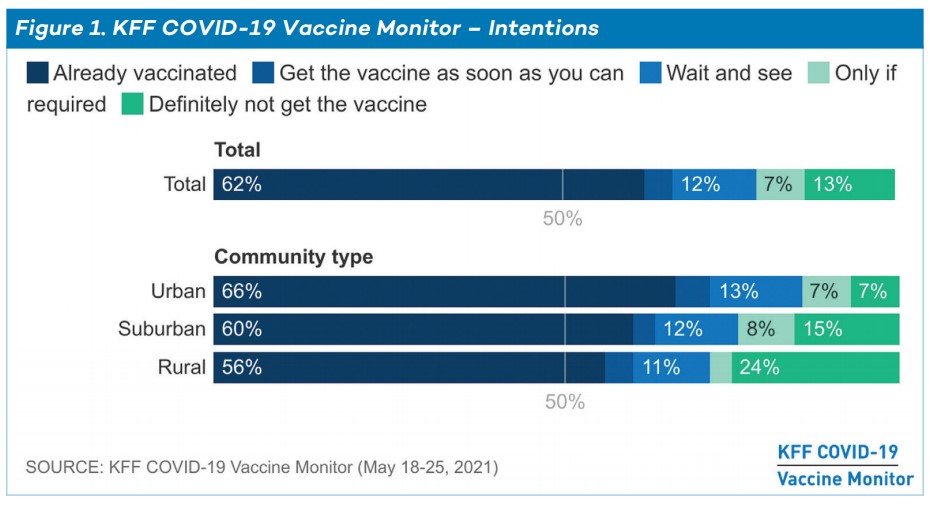
Vaccine hesitancy, or a lack of trust in vaccine safety, is a decades-long struggle in the United States. People who experience vaccine hesitancy often refuse vaccines or delay vaccination based on misinformation or safety concerns, which can include fears about side effects, lack of trust in government or the scientific establishment, and, particularly in the case of the COVID-19 vaccine, anxiety that it was developed too quickly. As of mid-May 2021, 32 percent of Americans were vaccine hesitant or vaccine refusers (12 percent “wait and see”, seven percent “only if required’ and 13 percent “definitely not”.)
There is not a one-size-fits-all approach to increasing vaccine confidence, as reasons for hesitancy depend on an individual’s personal experiences. However, evidence-based interventions exist, including engaging trusted community members and increasing public knowledge about the vaccine. Trusted community members can include medical professionals, religious leaders and others. Governors and state leaders can convene groups of trusted messengers to spearhead efforts to formulate community-wide plans for increasing vaccine confidence. Wyoming state health leaders, for example, have met with trusted community messengers for communities of color, disability rights groups and immigration rights groups to promote vaccine confidence through building long-term partnerships focused on equity. Other efforts in Wyoming include peer-to-peer panel discussions for clinicians led by local clinicians and a statewide provider champion network of school and public health nurses. In Maryland, the University of Maryland partnered with local barbershops and salons to hold vaccination events and to educate stylists on how to address vaccine concerns by equipping them with accurate medical information and to ensure stylists are equipped with accurate medical information regarding vaccine concerns.
Developing messaging strategies that reach people where they are is also important, especially in rural areas that may not have access to the Internet or other forms of media. State leaders have been creative in communicating about vaccine availability and education through TV ads, social media platforms, local radio stations, signs, posters, billboards and educational videos. For example, North Dakota Department of Healthsent out letters to those eligible for the vaccine during their phased allocation stage because many older adults and rural residents do not have access to the Internet or email. The letters included vaccine information and a hotline number to call to schedule an appointment. In states like California, Florida and Iowa, localities are holding vaccine events at county fairs where residents can receive accurate information and discuss their concerns.
Examples of Trusted Messengers
Trusted messengers are those within one’s own community or group, whether geographic or digital, that community/group members regard as credible sources of information.
- Local elected officials, e.g., mayors, state legislators, city council members
- Health care providers, e.g., family doctors, nurses, pharmacists, emergency medical technicians (EMTs), dentists, community health workers (CHWs), Federally Qualified Health Centers (FQHCs)
- Social services agencies and providers, e.g., social workers, counselors
- Faith leaders, e.g., pastors, imams, preachers, rabbis, priests, nuns, church administrators
- Educators, e.g., teachers, principals, school counselors, school nurses, school sports coaches
- Agricultural and industrial organizations, e.g., 4-H, Future Farmers of America, American Farm Bureau Foundation for Agriculture, National Farmers Union, United Mine Workers of America, National Association of Manufacturers
- Nonprofit organizations, e.g., Meals on Wheels, United Way, Boy and Girls Clubs, food pantries, state nonprofit associations, Salvation Army
- State and local chapters of professional societies, e.g., rural health associations
- Local businesses, e.g., barbers and hairstylists
- Mail and postal workers
Effective vaccine messaging requires community input so state and local governments and other stakeholders can address unique concerns in a culturally competent manner. Four in ten rural residents do not see the pandemic as a serious threat to the U.S. or their families, and 44 percent believe the news has “generally exaggerated” the seriousness of COVID-19. Studies have demonstrated the importance of avoiding the urge to correct false claims. This tendency creates divisiveness that further polarizes the issue. Collecting data on specific reasons underlying vaccine hesitancy is important for developing an effective strategy. For example, Utah’s Department of Health partnered with a state-based information technology firm to design a program to collect data from individuals getting tested for COVID-19 to determine why they might be hesitant to get the vaccine. This information will be used to design messaging.
Governors and state officials may consider the following when creating vaccine messaging campaigns:
Short-term strategies
- Establish avenues such as surveys, focus groups or town halls to hear from district, county and local leaders to understand the unique reasons for hesitancy within specific communities and develop targeted approaches.
- Include trusted community members to be the conduit of information.
- Provide consistent information to the public through coordinated state and local messaging campaigns.
- Create a unified, bipartisan message to resonate across ideological lines and unites state and local leaders on vaccine and public health messaging.
- Identify trusted community voices to combat vaccine misinformation and answer questions of their peers through groups like health neighborhoods and immunization coalitions.
- Conduct outreach through multimodal communication such as Facebook Live, radio station programming (FM and AM), weekly town halls, or repurpose messaging platforms used to reach voters and send census reminders.
Long-term strategies
- Encourage organizations and state agencies to fold in vaccine education information to other public health campaigns and community programs, e.g., parenting classes or substance use disorder treatment.
- Establish groups of trusted community voices throughout the state to engage in public health messaging beyond COVID-19.
Consideration 2: Establish straightforward pathways for individuals in rural areas to access vaccines within their communities.
To meet the health care access challenges that many people in rural areas experience, Governors can invest in models of care that bring health care services outside of the clinic and into the community including community paramedicine, mobile clinics and home-based care. States can also increase transportation access in rural communities through partnerships with public transit systems, ride-share companies and state departments of transportation. Changes to scope of practice and flexibilities for non-clinical providers can also increase access to vaccine and other needed health care services, important for rural communities, which are more likely to have health professional shortage areas.
States have expanded vaccinations beyond the clinical setting in several ways during the Public Health Emergency. Using paramedicine or emergency medical services (EMS) professionals allows for easier vaccine delivery to those that are homebound. States have amended Medicaid plans and worked with commercial insurers to reimburse for some of these services, as there are barriers for reimbursement of EMS services that do not end with a transfer to a hospital. Minnesota was the first state to allow EMS to bill Medicaid for community paramedicine services. Indiana used a partnership approach between the Department of Health Homebound Hoosiers program and EMS services. The program pairs EMS workers with high-risk, homebound individuals who want the vaccine to administer the vaccine and observe the patient in their own home. Another method is the use of mobile or pop-up clinics which can be quickly set up for brief periods of time. The South Carolina Department of Health deployed mobile COVID-19 vaccine vans to rural and underserved parts of the state. The vaccination units were set up at small businesses, recreation centers, parks and in the vehicles themselves, making it convenient to get vaccinated.
To further increase access, Governors are partnering with state and local transit systems, ride-share companies and their state departments of transportation to bring individuals to vaccination sites. Kentucky, Mississippi, Michigan, North Carolina and Ohio allocated funding to provide free or reduced-cost transportation across the state for those who want to be vaccinated but may be unable to get to a site. Local efforts across 47 states are also providing free or reduced-fare trips to and from vaccination sites. Similarly, state, territory and local governments have partnerships with rideshare companies to provide free on-demand rides.
Furthermore, state scope-of-practice laws vary on which providers are eligible to administer vaccines. Each state has unique scope-of-practice laws for vaccines, including which type of vaccine a provider can give, the age range for which a vaccine can be administered, requirements for parent/guardian approval and supervision provisions. The Public Health Emergency prompted many states to temporarily expand the vaccine scope of practice for health care providers including nurse practitioners, physicians’ assistants, pharmacists and others to increase capacity of the existing health care delivery system. Although these flexibilities were temporary, Governors may consider evaluating the impact that such changes have and determine if they could increase access to services moving forward. For example, Louisiana’s Department of Health issued a protocol allowing EMTs to administer vaccines during the current and future public health emergencies by providing flexibility with their language, stating that licensed EMS professionals at the EMT and Advanced EMT levels can administer vaccines related to a declared Public Health Emergency/event and/or disaster.
Scope of practice: Activities and procedures that a person with a specified level of education, training, and competency is authorized to engage in under the statutes and regulations of the state in which the person practices. States and regulations may incorporate conditions that limit the exercise of authorized activities and procedures.
In addition to flexibility for licensed health care providers, states may consider ways of supporting the workforce responsible for the non-clinical aspects of vaccine administration. Patient education, counseling and coordination are crucial to ensuring a more streamlined, efficient vaccine administration process. For example, State Medical Reserve Corps were an important method of recruiting volunteers for various tasks such as health education and counseling, setting up appointments and monitoring people after vaccine doses were administered. Virginia Governor Ralph Northam issued a call for volunteers for both medical and non-medical professionals to help coordinate the vaccine rollout. The announcement specified opportunities for further training, such as basic medical skills, transferring to intensive care or medical-surgical units and using ventilators.
Obtaining vaccine access also includes the ability to retrieve information on how and where to get the vaccine.The Minnesota Vaccine Connector, a statewide tool run through the Department of Health, connects patients with vaccinators. The website allows individuals to search vaccine locations and determine their eligibility with the option to register for updates. For those unable to make appointments online or needing assistance, the state also set up a hotline. West Virginia developed vaccine safety and availability resources specifically for health care providers including example social media posts, printable infographics, newsletter templates and other materials. The resources were developed with the Governor’s office, the West Virginia Department of Health and the National Guard. The state also developed a list of best practices like high-traffic times to make posts, making images accessible for people with disabilities and positive social media engagement.
Non-Emergent Partnerships
States leveraged partnerships with organizations specializing in the training and deployment of health care professionals during the Public Health Emergency. One of the programs states used is known as an Area Health Education Center (AHEC).
With more than 300 programs, an AHEC’s goal is to train and deploy qualified health professionals to rural and underserved communities. The Alabama Department of Public Health partnered with the state AHEC office to set up five regional vaccination sites. By using the existing network at the University of Alabama at Birmingham, the Department was able to quickly deploy qualified vaccinators to underserved areas in the state.
Short-term strategies
- Explore models for vaccination outside of the clinical setting, including home vaccinations, mobile vaccination units, and community paramedicine.
- Expand access to vaccine sites through transportation partnerships.
- Institute a variety of ways to disseminate registration, availability, and update information to the public, including social media, press conferences, hot lines, provider networks, etc.
Long-term strategies
- Expand scope of practice laws to increase pool of health care workers who can vaccinate.
- Provide rural areas with the opportunity to recruit and leverage nonclinical providers to support work including but not limited to community health workers, medical reserve volunteers, peer coordinators and National Guard members.
- Invest in rural workforce by leveraging partnerships and coordinating with existing organizations who specialize in recruitment and retention of the public health workforce, such as community health worker associations, community colleges and training centers.
- Conduct a workforce study to understand the health care workforce gaps in the state and where investments are needed.
Consideration 3: Develop and streamline sustainable systems to strategically allocate and distribute vaccines to rural and frontier populations.
COVID-19 vaccine distribution has been an unprecedented challenge for public health systems. Complications related to storage and handling, equitable allocation and issues with interoperability between data systems complicated transferring millions of doses from the manufacturers to providers. Rural and frontier areas faced unique challenges managing distribution such as transportation, large shipments, long distances and lack of broadband. Governors and state officials have worked to address these issues by revamping existing data collection systems or creating new ones. Federal funding has provided necessary resources, and now there is a question of ensuring sustainability and further modernization of these systems and strategies.
Prior to emergency use authorization of a COVID-19 vaccine, states were required to develop plans for when one or more became available. The plans included allocation and distribution strategies among other components. For example, Alaska uses a regionalized model to distribute vaccine shipments. The vaccine allocation is received at the Anchorage airport and then is divided and transferred to smaller depots throughout the state. The packages are reduced to smaller quantities to decrease wastage and then sent to health care facilities and vaccine clinics. Georgia has a similar practice where vaccines are shipped to a Department of Public Health warehouse and broken down to as few as 60 doses then transported to vaccine clinics by state patrol officers and other state employees. In addition to redistribution of vaccines, other resources crucial to vaccine distribution have been shared among localities such as personnel and vehicles to transport individuals to vaccination sites. In Wyoming, the University of Wyoming provided surge personnel and conducted vaccination efforts for the community with other public health partners, and Department of Health strike teams supported vaccination efforts within many communities. Similarly, in Rooks County, Kansas the community came together to pool resources. The local hospital received vaccines and redistributed to its affiliates and independent practices, and residents volunteered to help, making the initial phases of vaccine distribution a community-wide effort.
Governors and state officials may consider the following when strategizing around allocation and distribution of vaccines to rural and frontier populations:
Short-term strategies
- Establish distribution centers to break up large shipments of vaccines and/or supplies and deliver compatible quantities to areas with smaller populations.
- Use data systems and mapping to create systematic vaccine distribution streams to rural, frontier, and socially vulnerable areas.
- Encourage district, county, and locality to connect and share resources including:
- Mobile medical vans to serve as mobile vaccine clinics
- Resources from community-based organizations, such as church vans or unused school buses for transporting individuals to and from vaccine sites
- Additional personnel to administer vaccine or volunteer at vaccine sites such as: emergency medical services, medical students, community health workers and the National Guard
Long-term strategies
- Increase flexibilities with reimbursement or transportation funding to expand mobile vaccine strategies, such as the use of emergency medical service personnel, beyond the COVID Public Health Emergency.
- Automate reporting to state immunization systems through electronic medical records to improve reporting efficiency and timeliness of reporting.
- Establish an office that brings together state employees from all areas of public health to collaborate and coordinate resources to implement comprehensive, data driven strategies that promote equal access to high quality health care and control costs.
Louisiana Vaccine Strategy
Louisiana took a multi-pronged, unique approach to increase vaccine uptake, especially in rural communities. Using Coronavirus Aid, Relief, and Economic Security Act (CARES Act) funding, the Louisiana Department of Health developed a mapping system with ArcGIS – a mapping and analytics software – using census tract data to identify gaps in vaccination access based on the social vulnerability index (SVI), high COVID-19 case and/or death rates and low vaccination rates. Using the layers in the mapping system, regional medical directors in the state determined a vaccine allocation formula, sending vaccines to areas highest on the SVI with the lowest vaccination rates, which were typically rural communities. These data were updated weekly to ensure equitable allocation throughout the state. In areas with a dearth of available vaccinators, the state sent “hot shot teams” made up of National Guard members to administer the vaccines. Using vaccine serial numbers, the mapping system is now incorporating vaccine expiration date data to determine those that can be redistributed by hot shot teams to minimize wastage.
Louisiana, like the rest of the country, saw a drop in demand as vaccines became more widely available. To increase uptake and respond to hesitancy and concerns, the Vaccine Equity Project was formed as part of Bring Back Louisiana, the state’s campaign to get vaccines out to communities. The effort is a partnership between Together Louisiana, the Louisiana Department of Health, the Louisiana Public Health Institute, Louisiana Primary Care Association, vaccine providers, the Power Coalition and other community organizations. Also funded through CARES, the Vaccine Equity Project pays canvassers $15 an hour to go door-to-door in neighborhoods identified through the mapping system to share information and register individuals for vaccine appointments. After spending several days canvassing, a vaccine clinic event is held in the neighborhood for residents.
Next Steps
Given the influx of federal funding during the Public Health Emergency, Governors have the opportunity to bolster their public health systems, especially in rural areas. The American Rescue Plan Act (ARP) and the Coronavirus Aid, Relief, and Economic Security Act (CARES Act) allocate funds to rural-specific COVID-19 responses and provide states and territories flexibility to finance initiatives to modernize existing data and information systems or invest in strategies to create broad access to health care. For example, the Health Resources Service Administration (HRSA) received ARP funding to create both the Rural Health Clinic Vaccine Confidence Program and Rural Health Clinic COVID-19 Vaccine Distribution Program. Both are designed to reach rural areas either through messaging or getting vaccine into hard-to-reach areas. HRSA also provided $398 million to the Small Rural Hospital Improvement Program to maintain or increase COVID-19 testing, expand access to testing for rural residents and tailor mitigation efforts to reflect the needs of local communities at 1,540 rural hospitals. Another prevention and screening effort through HRSA, the Rural Health Clinic COVID-19 Testing and Mitigation Program, provided $460 million to support 4,600 rural health clinics to maintain and increase COVID-19 testing efforts while expanding access to testing and scaling up mitigation activities in rural communities. States can use both CARES and ARP to address current vaccination efforts. For example, Nevada allocated CARES funding to support enhanced vaccination media campaigns focused on reduction of respiratory illnesses, including COVID-19 and influenza. Idaho used its funding to enroll and train providers in COVID-19 vaccine administration.
Governors have also used this funding to address challenges that have affected access to preventative services in rural areas such as broadband and workforce shortages. Limited Internet access impedes rural providers from using electronic medical records or providing telehealth services. Several states, including Hawai‘i, Idaho, Iowa, Maine, Missouri, North Carolina, Oregon, Utah, Vermont, West Virginia and Wisconsin used CARES funding to expand broadband and telehealth access to rural areas. Additionally, the pandemic highlighted the importance of the public health workforce and prompted significant investments at the federal and state levels. Not only will there be opportunities to fund training and retention programs, but there are many professionals who were expeditiously recruited and trained during COVID-19 such as peer coordinators, contact tracers, case managers, and other professionals who could remain in the sector.
Conclusion
Governors serve an important role in addressing COVID-19 vaccine access and uptake throughout their states and especially in rural communities where confidence is very low. Strategies outlined in this paper can help address many of the issues; however, Governors will need to ensure sustainability to build back trust and create better systems for the future. Partnerships with rural stakeholders will be paramount not only to increase uptake, but also to inform how Governors can build on progress and establish a strong public health infrastructure for these communities.
Acknowledgements
NGA Center would like to acknowledge and thank national experts and state officials who granted informational interviews, reviewed drafts and provided content for this publication. The NGA Center would also like to thank the Health Resources and Services Administration and the Federal Office of Rural Health Policy for their generous support through the duration of this project, especially during the creation of the project.
Recommended Citation Format
LeBlanc, M., Ruane, K.*, Fairbanks, M.*, & Roy, B. (2021 July). State Strategies to Increase Vaccine Uptake in Rural Communities. Washington, DC: National Governors Association Center for Best Practices.
*Kelsey Ruane and Molly Fairbanks contributed to the development of this report during their tenure at the NGA Center.













