This issue brief includes key considerations regarding state strategies to address type 2 diabetes prevention and diabetes management.
Introduction
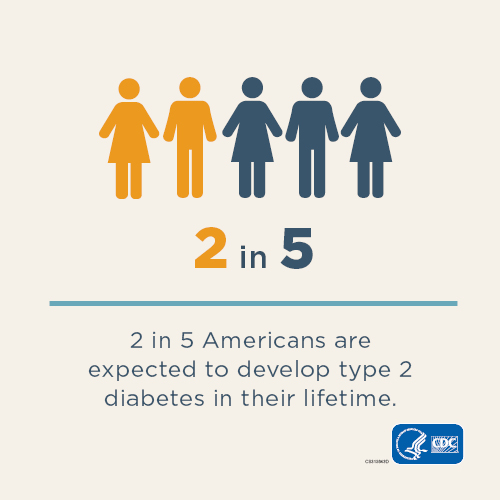
More than 34 million people in the United States—1 in 10—have diabetes, and most of these people have type 2 diabetes, which is preventable. In addition, a staggering 88 million U.S. adults—about 1 in 3—have prediabetes, a serious health condition where blood sugar levels are elevated but not as high as in people with diabetes. In terms of cost, the Centers for Disease Control and Prevention (CDC) estimates that $1 out of every $4 of U.S. health care costs is spent on caring for people with diabetes.
Though access to clinical care and behavioral choices are central to type 2 diabetes prevention and diabetes management, factors including educational attainment, income, housing stability, access to nutritious food, and employment security—known as social determinants of health (SDOH)—have a profound effect on health outcomes, including the likelihood of developing type 2 diabetes. Conventional type 2 diabetes prevention and treatment strategies focus on clinical treatment combined with behavioral modifications, such as adoption and maintenance of increased physical activity and healthful eating. However, these strategies do not take into consideration the impact of poverty and material deprivation, which can lead to chronic stress and amplify the likelihood of engaging in unhealthy behaviors, which in turn increases the likelihood of developing obesity and type 2 diabetes.
Racial and ethnic minorities and low-income populations are disproportionately affected by prediabetes and type 2 diabetes. In 2018, 12.5 percent of Hispanic or Latino persons, 9.2 percent of Asian persons, 14.7 percent of Native American or other Pacific Islander Persons, and 11.7 percent of non-Hispanic Black or African persons had diagnosed diabetes, compared to 7.5 percent of White persons. Social and economic conditions contribute to the racial and ethnic health disparities observed in the development of chronic diseases like type 2 diabetes. This is in part due to the increased frequency of interrelated social and economic conditions such as reduced access to health insurance coverage, stable housing and employment, and healthy food in communities of color.
Over the past year, the COVID-19 pandemic has exacerbated existing challenges related to food, housing and employment-related hardships. Furthermore, people with diabetes, though not at additional risk of contracting the virus, are more likely to develop serious complications and die from COVID-19. The COVID-19 pandemic has led many individuals to delay standard care and forego appointments and procedures. For patients with or at risk of diabetes, access to consistent, quality health care is crucial to successfully managing their condition.
To reduce the incidence of type 2 diabetes across the nation, approaches must apply a comprehensive social-ecological framework, incorporating not only intensive individual lifestyle interventions but also policies and programs to enable neighborhoods, workplaces and other environments to contribute to lasting behavioral change. This is particularly critical during the pandemic, as social support networks, which are known to promote healthier behaviors and positive health outcomes (particularly in lower-income communities), have been frayed and rates of isolation and loneliness have risen. Critical to type 2 diabetes prevention and diabetes management are interventions intended to create greater access to non-medical resources that address social needs linked to health and health outcomes.
On January 21, 2021, the National Governors Association Center for Best Practices (NGA Center), with the support of the Centers for Disease Control and Prevention, convened national and state experts in a discussion about state strategies to address type 2 diabetes prevention and diabetes management. This issue brief includes key considerations emanating from the expert roundtable and associated research.












