This brief describes innovative approaches and communication strategies states and territories are using to address health equity needs.
(Download)
Governors are leading the way in addressing health equity in their states and territories to reduce health disparities across multiple areas. For the last year, the National Governors Association Center for Best Practices (NGA Center) explored ways states and territories are addressing and communicating about health equity across and within these areas. This includes reducing health disparities for people with disabilities, people of all races and ethnicities, and among rural populations. Through desk research, learning calls, and convening states and territories in roundtable discussions, the NGA Center gathered promising strategies for this work from examples shared by state and territory leaders. This brief includes information on several of these strategies as examples of how state and territory leaders can create effective health equity approaches and communication strategies that can contribute to dynamic health equity plans.
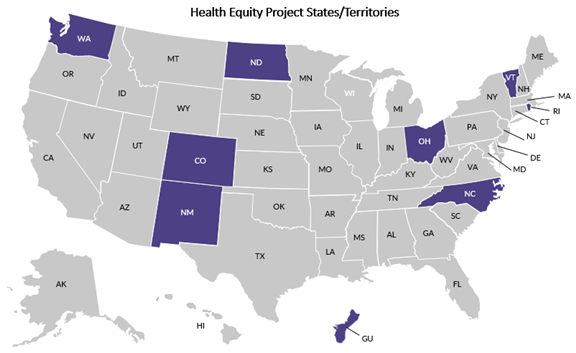
The project began with NGA staff conducting desk research and learning calls with states and territories. The NGA Center conducted an environmental scan of Governors’ approaches and structures to organize health equity efforts. The NGA team also spoke with staff in over a dozen states and territories to gather information on innovative health equity strategies through a series of learning calls. Based on these calls, the NGA Center identified a group of nine states and territories with innovative health equity practices across the three identified areas of focus to work with as part of this one-year project. These states and territories are geographically and politically diverse and have varied health equity goals reflecting the needs of their unique populations.
The NGA Center held a virtual workshop on March 23, 2023, with this group of states and territories to support peer learning and sharing of health equity successes and challenges. Attendees joined from the following states and territories: Colorado, Guam, New Mexico, North Dakota, Ohio, Rhode Island, Vermont and Washington. Workshop discussion topics included: framing health equity initiatives, structuring health equity work, legislative and policy assessment models, working with community-based organizations, and health care provider and network cultural responsiveness requirements and design.
The NGA Center also held an in-person roundtable in Broomfield, Colorado, August 24, 2023, that brought together eight project states and territories as well as Wisconsin, a state interested in NGA’s health equity project. Participants discussed communication strategies Governors and their staff can use to message about health equity in rural communities and how this can apply more broadly to other populations. Other session topics included centering disability in health equity approaches and integrating equity into the policymaking process. State teams also had time to discuss health equity goals and action plans. Next steps for the state attendees included sharing these priorities and outcomes from the roundtable with colleagues in the Governor’s office and in other agencies.
The NGA team compiled information from discussions in these convenings as well as in learning calls and research to identify high-level themes and insights. The three themes that emerged as top health equity priorities for states are:
- Coordinating health equity initiatives across agencies,
- Centering community voice and priorities in health equity work, and
- Integrating equity into policymaking.
The remainder of this brief describes innovative state and territory examples within these three themes.
COORDINATING HEALTH EQUITY INITIATIVES ACROSS AGENCIES
Colorado: In Colorado, the Governor’s office organizes multiple initiatives to contribute to a cohesive health equity vision. NGA Vice Chair Colorado Governor Jared Polis issued Executive Order 175 in 2020 to direct state agencies to integrate equity in systems, policies and practices through activities such as training and participation in the Colorado Equity Alliance. State initiatives supporting health equity include:
- The Office of Saving People Money on Health Care: This office, overseen by Colorado Lieutenant Governor Dianne Primavera, aims to identify and address the root causes of the high costs patients face.
- All Roads Lead to Health Cabinet: Lieutenant Governor Primavera also oversees this cabinet, which coordinates health equity efforts across state government. Lieutenant Governor Primavera spoke about this initiative at NGA’s health equity roundtable held in August 2023.
- Colorado Equity Alliance: This initiative includes members from state agencies and community organizations focused on making state government more equitable. This includes making state government spaces and activities fully accessible to people with disabilities.
- Colorado Option: The Colorado Option is a state-designed insurance plan that aims to reduce insurance costs and increase culturally responsive provider networks. These networks must include health professionals who reflect the diversity of the plan’s enrollees in terms of race, ethnicity, gender identity and sexual orientation.
- Equitable Budgeting: Governor Polis’ Office of State Planning and Budgeting asks state agencies to describe how budget requests promote equitable outcomes (see page six of this brief for more information).
Edwin Chen, Health Policy Coordinator in Governor Polis’ office, presented on these efforts at NGA’s Health and Human Services Policy Advisors Institute held in October 2023.
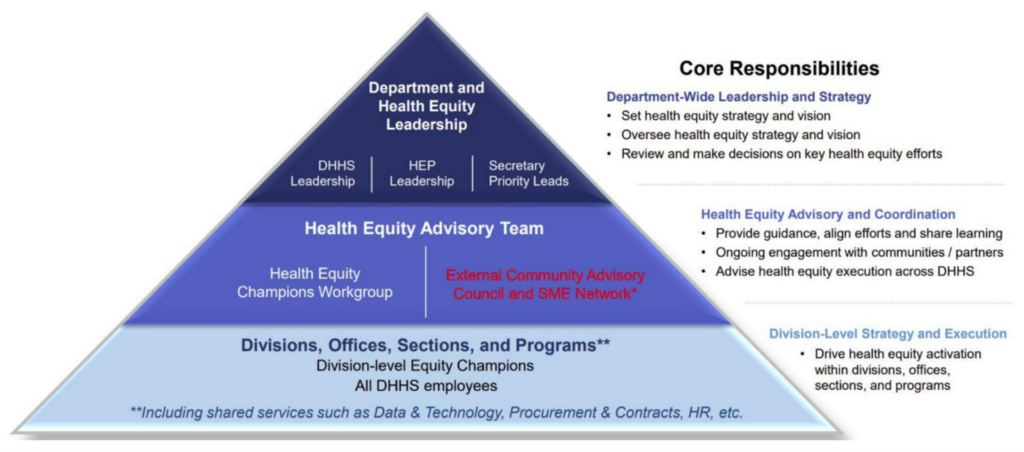
North Carolina: In 2021, the North Carolina Department of Health and Human Services (NCDHHS) created the Chief Health Equity Officer role to lead the state’s health equity work. The Chief Health Equity Officer provides unified leadership over both internal and external strategies to address health disparities for historically marginalized populations. This position coordinates a health equity portfolio comprised of the Offices of Rural Health, Diversity, Equity, and Inclusion, Olmstead/ADA and Health Equity. In addition to providing leadership and a health equity vision to the rest of the department, the Chief Health Equity Officer and their team provide tools, templates, consultation and resources for communities and NCDHHS teams to implement or evaluate health equity approaches in their work.
The NCDHHS also created a Health Equity Governance Model to define the department’s health equity responsibilities and leadership structure. This model was developed based on interviews with NCDHHS division leaders, a survey issued to department employees and a review of governance structure models from other states.
Washington: In Washington, the Governor’s Interagency Council on Health Disparities provides recommendations to the Governor and the legislature to eliminate health disparities by race, ethnicity, and gender in the state. The council was established by legislation in 2006, and members represent state agencies, boards and commissions, as well as the Governor’s office. The council holds public meetings, convenes advisory committees focused on specific health equity issues and contributes to Health Impact Reviews along with the State Board of Health. These reviews are assessments of how proposed legislation would impact health and health equity in the state. One priority the council adopted is to implement the National Standards for Cultural and Linguistically Appropriate Services (CLAS Standards). The adoption of these standards can support improved access to health care services and information.
Washington also has an Environmental Justice Council that works to advise state agencies on incorporating environmental justice into their work. The council defines environmental justice as “the fair treatment and meaningful involvement of all people regardless of race, color, national origin, or income with respect to the development, implementation, and enforcement of environmental laws, rules, and policies.” The council’s work aligns with the Healthy Environment for All Act (HEAL), the first statewide law to create a coordinated and collaborative approach to environmental justice, making it a priority and part of the mission of key state agencies. The law requires certain agencies to identify and address environmental health disparities in overburdened communities and for vulnerable populations.
Samantha Pskowski, Policy Advisor for Public Health in Washington Governor Jay Inslee’s Office, presented on Washington’s approach to health equity in NGA’s virtual workshop in March 2023.
Wisconsin: The Wisconsin Governor’s Health Equity Council works to address factors contributing to health disparities in the state. Wisconsin Governor Tony Evers established the council through Executive Order 17 in 2019 with the directive to develop a comprehensive plan to reduce and eliminate health disparities in the state by 2030. The council released a report in January of 2023, “Building a Better Wisconsin: Investing in the Health and Well-Being of Wisconsinites,” to issue recommendations to address economic, social and physical environmental factors related to health. Several recommendations from the report were incorporated in the Governor’s budget, such as funding the Workforce Housing Rehabilitation Loan Program to provide low interest and forgivable loans to lower income households for lead remediation and other repairs. The final budget included $50 million for this program to support equitable housing.
CENTERING COMMUNITY VOICE AND PRIORITIES IN HEALTH EQUITY STRATEGIES
Guam: Health equity is a top priority for Guam Governor Lou Leon Guerrero. Guam promotes health literacy and cultural humility to increase health care access through health care worker training. The territory’s Office of Minority Health (OMH) employs CLAS standards to train health care providers to deliver culturally and linguistically appropriate care. The territory faces health care workforce shortages and recruits workers from neighboring countries to fill the gap. These people may speak different languages and have cultural differences from their patients in Guam. The OMH training helps new health care workers gain the skills to communicate effectively and appropriately with patients.
Alex Silverio, Program Coordinator for the Guam Department of Public Health and Social Services, presented on Guam’s cultural responsiveness training in NGA’s virtual workshop in March 2023.
New Mexico: In New Mexico, the Governor’s office worked with theNew Mexico Department of Health (NMDOH) to develop a State Health Improvement Plan (SHIP) with a focus on health equity to work across state agencies, community organizations, and tribes, pueblos, and nations. The SHIP seeks to align with executive priorities, as well as community priorities, to develop policies and programs that promote health, coordinate resources and measure progress.
The Governor’s office, NMDOH and other state agencies created the framework below to illustrate the SHIP development process. The first phase is focused on building the plan’s foundation, including: 1) building a health equity data unit to collate data across agencies to share with communities to identify priorities and 2) assembling and training a facilitator team to work with communities to share and utilize data and develop community health assessments. Phase two is focused on aligning data from the state health assessments and community health assessments across the state. New Mexico is now in the third phase of the SHIP process and continues to convene partners to address the key priorities of the SHIP and to collaboratively take action to improve equity outcomes.
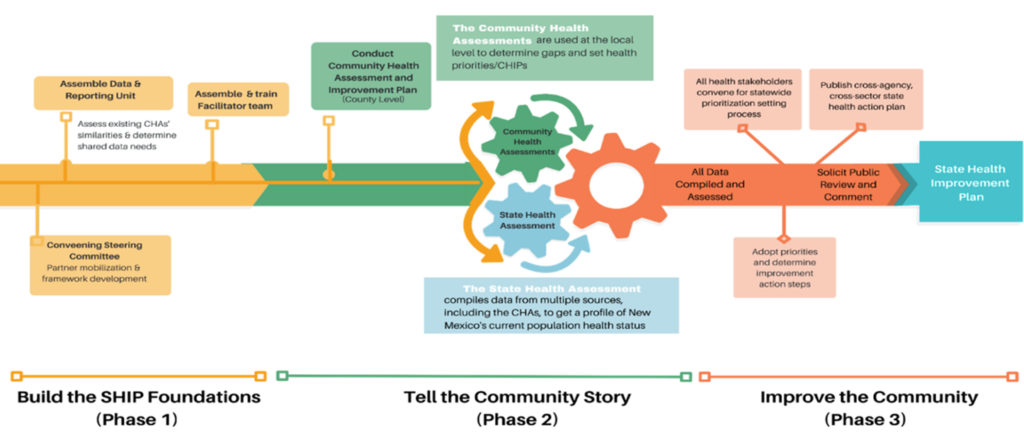
With a combination of state general funds and federal funding from the Centers for Disease Control and Prevention (CDC), the Governor’s office and NMDOH developed an equity-focused SHIP with funding for community organizations, tribes, pueblos, and nations to meaningfully participate in the SHIP development. New Mexico engaged coordinators to guide and lead the work, epidemiologists to gather health equity data for communities and state agencies to review, and provided funding for tribes, pueblos, and nations to have summits to give feedback and further suggestions to the SHIP. NMDOH, in coordination with the Governor’s office, continues to convene SHIP meetings and participated in a health equity summit convening with multi-sector partners in collaboration with the University of New Mexico in 2022. This summit will be held again in December 2023.
Dr. Laura Parajon, Deputy Secretary of the New Mexico Department of Health, presented on New Mexico’s approach to health equity in NGA’s virtual workshop in March 2023.
North Dakota: North Dakota’s Community Engagement unit within the Department of Health and Human Services (NDHHS) leads the state’s work in reducing health disparities. The Community Engagement unit’s primary goal is to work alongside North Dakota communities in addressing health-related needs to reduce disease rates by providing opportunities for interventions and improving access to health care. The team’s name reflects the work this group does to partner with communities in the state.
One such community is the American Indian tribes of North Dakota, including the Mandan, Hidatsa, and Arikara Nation, the Spirit Lake Nation, the Standing Rock Sioux Tribe, the Turtle Mountain Band of Chippewa Indians, and the Sisseton-Wahpeton Oyate Nation. The Community Engagement unit includes four tribal health liaisons who work to bridge communication between NDHHS and tribal communities and surrounding urban areas while addressing and improving tribal health equity. Each tribal health liaison is primarily assigned to one or more tribes, with two liaisons covering the Eastern and Western regions of the state and providing backup to each other. Tribal health liaison activities include: education and awareness of COVID-19, including testing and addressing vaccinations to tribal partners; collaboration with various state and local programs and entities to provide expertise, resources and support (e.g., family planning, oral health, behavioral health, veterans affairs, schools, health care systems, urban homeless shelters, rape crisis centers, food pantries) around tribal health needs; serving as content experts on task forces, committees, coalitions, etc.; assisting with tribal efforts to promote healthy pregnancies and postpartum care; and education and awareness of infectious and chronic diseases to tribal partners. Fostering working relationships with each of the five tribes is a critical work function of the tribal health liaisons and the Community Engagement unit. This work is rooted in communication, cultural awareness, and respect and understanding.
Krissie Gerard, Community Engagement Director, and Kim Mertz, Healthy and Safe Communities Section Director, both from the North Dakota Department of Human Services, presented on the Community Engagement unit in NGA’s virtual workshop in March 2023.
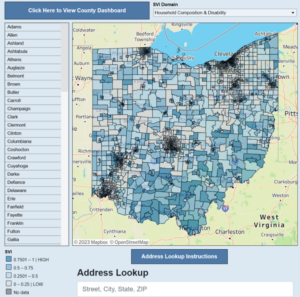
Ohio: In Ohio, community is at the center of state health equity initiatives. The Ohio Department of Health (DOH) operates the Ohio Health Improvement Zones program to advance health equity in communities across the state. Health Improvement Zones are areas identified as having socioeconomic and demographic factors contributing to a higher social vulnerability score. The CDC developed the SVI to measure social determinants of health, such as poverty or lack of access to transportation, at the community level. In 2022, the Ohio DOH awarded $6.9 million to 26 community based organizations (CBOs) to support health equity in health improvement zones. This program is rooted in data and the DOH created a publicly accessible mapping tool to illustrate Social Vulnerability Index (SVI) scores at the census tract level.
The Ohio DOH is piloting a CBO Resource Center to provide support in grant writing and financial sustainability to CBOs in the state. The resource center helps CBOs build capacity by providing these organizations with shared services and consultative services. Ohio is piloting this program in an urban community and in an Appalachian community.
Jamie Carmichael, Assistant Director of Community Planning and Collaboration at the Ohio Department of Mental Health and Addiction Services, presented on Ohio’s Health Improvement Zones in NGA’s virtual workshop in March 2023.
INTEGRATING EQUITY INTO POLICYMAKING
Colorado: The Colorado Office of State Planning and Budgeting within the Governor’s Office started integrating equity into the budgeting process in 2020. The Budgeting Office asks state agencies to describe how budget requests promote equitable outcomes. This process is intended to ensure funding allocations directly address historical inequities, increase opportunities for marginalized groups and promote prosperity for all Coloradans. State agencies are asked to identify historically underserved groups affected by the request, describe existing equity gaps and explain how the request affects these gaps. The state is continuing to implement this process and evaluate budget outcomes.
Manny Santistevan, Senior Budget and Policy Analyst in the Colorado Governor’s Office of State Planning and Budgeting, presented on this initiative at NGA’s health equity roundtable in August 2023.
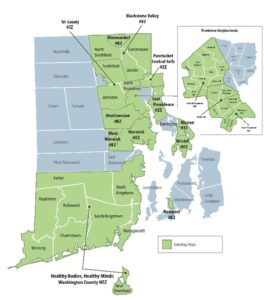
Rhode Island: In Rhode Island, a whole of government approach is taken to advance health equity. The Department of Health developed Rhode Island Health Equity Measures in conjunction with the Community Health Assessment Group to help the state track determinants of health across the state. These measures come from several state and federal sources and fit into the following domains: integrated health care, community resilience, physical environment, socioeconomics and community trauma. This data is used to inform statewide efforts to identify and improve upstream social, environmental, and economic inequities in communities across Rhode Island. Using Geographic Information System technology to map the Health Equity Measures geospatially, Rhode Island’s Health Equity Zone (HEZ) initiative leverages these data to create community profiles for each of the Health Equity Zones to support the equitable deployment of resources to improve the Equity Measures in each HEZ community. Through this approach, Rhode Island has aligned environmental justice, housing development, public health, Medicaid, behavioral health, economic development, civic engagement, emergency response, health care access and other state investments directly with the communities who need them most.
Chris Ausura, Director of the Health Equity Zones Initiative in the Rhode Island Department of Health, presented on the state’s approach to health equity in NGA’s virtual workshop in March 2023.
Vermont: Vermont’s Office of Racial Equity developed a Policy Impact Assessment to use as a framework for the development and review of a proposed policy in the executive branch. This tool assesses the direct and indirect potential impacts of proposed policies, with the goal of shaping policies and budgets to advance equity.

The tool includes questions to assess the policy proposal’s impact, as well as an introductory section and a reference section. The reference section includes a glossary of defined terms, such as “equity” and “performance measure,” frequently asked questions, and linked resources for further learning. The impact assessment itself includes questions organized into the following sections: background, problem definition, proposal, stakeholders and impacts, resources, and measurement and monitoring.
The tool is intended to be used at the beginning of policy development to ensure equity is considered and integrated throughout the development process. The impact assessment may also be used to inform project planning and to assess existing legislation, policies, and programs.
This tool has been used in Vermont since 2021, and the Office of Racial Equity has several lessons learned from fielding the tool. First, they realized the importance of providing clarity and transparency on the tool’s purpose are key for getting state agency staff buy-in. By explaining the value of integrating equity into the policymaking process, state agency staff will understand that their input and equity analyses have an impact on reducing disparities in the state. Second, they created a streamlined tool in an accessible format to improve the experience of using the assessment. Third, they learned they need to provide enough time and training opportunities for staff to learn and adjust to the new process.
Vermont’s Office of Racial Equity will continue to evaluate outcomes from using the tool to understand how best to advance equity in the state. Vermont made information and training related to the tool public and presented on the tool at several convenings, aiming to share this model with other states. Xusana Davis, Vermont’s Executive Director of Racial Equity, presented on the tool at NGA’s virtual workshop in March 2023 and at the health equity roundtable in August 2023, and Monica Hutt, Vermont’s Chief Prevention Officer, presented on the tool at NGA’s Health and Human Services Policy Advisors Institute in October 2023.
Conclusion
Discussions with states and territories revealed best practices and innovative initiatives in addition to future priorities. Going forward, states and territories are focused on working with community based organizations to carry out health equity work and supporting these organizations through sustainable funding and training in financial management. Bringing disability equity more fully into the health equity conversation is also a priority. This includes improving the collection of disability health data and using this information to better understand the challenges this population faces. States and territories also identified the need for a shared common terminology when it comes to health equity. The NGA Center will continue working on these issues for the next two years with the Robert Wood Johnson Foundation on a new project entitled State Approaches to Cross-Cutting Health Equity Policies that will aim to create a health equity learning network, identify best practices for policy development and implementation related to intersecting areas of health equity, and support state technical assistance needs. For more information on this project or other health equity research or technical assistance, contact Anna Heard, Senior Policy Analyst, at aheard@nga.org.
Acknowledgements
The NGA Center would like to thank the Robert Wood Johnson Foundation (RWJF) for their generous support for development of this publication and the associated health equity project, State Efforts to Address and Communicate Best Practices on Health Equity. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the views of RWJF.
This paper was developed by Anna Heard in collaboration with Program Director, Shelby Hockenberry, and in consultation with RWJF Senior Policy Officer, Elizabeth DiLauro. The NGA Center would like to thank the state officials and other experts whose expertise contributed to this publication as well as the NGA staff who contributed expertise and review of this publication.
Recommended Citation
Heard, A and Hockenberry, S. Leading State Approaches Leading State Approaches and Communication Strategies to Support Health Equity. Washington, DC: National Governors Association, December 2023.
Figure Sources
- Figure 1: “Health Equity Call for Action,” State of North Carolina Department of Health and Human Services, accessed October 10, 2023, https://www.ncdhhs.gov/divisions/office-health-equity/health-equity-call-action.
- Figure 2: “New Mexico SHIP Process Framework,” State of New Mexico Department of Health, accessed December 6, 2023.
- Figure 3: “Health Improvement Opportunity Zones,” State of Ohio Department of Health, accessed October 10, 2023, https://odh.ohio.gov/know-our-programs/health-equity/health-improvement-zones.
- Figure 4: “Rhode Island Health Equity Zone Initiative,” State of Rhode Island Department of Health, accessed December 12, 2023, https://health.ri.gov/programs/detail.php?pgm_id=1108
- Figure 5: “State of Vermont Policy Impact Assessment,” State of Vermont Office of Racial Equity, accessed October 10, 2023, https://racialequity.vermont.gov/sites/reap/files/doc_library/SOV%20IA%20Tool%20%5BRev%202022-08-18%5D.pdf.