This paper contains best practices to best position healthcare facilities when energy stressor events occur, prioritizing healthcare facility energy resilience.
(Download)
Introduction
Over the past several years, the National Governors Association Center for Best Practices (NGA Center) has supported states and territories on issues related to the healthcare workforce. Much of this work has focused on supporting and recruiting healthcare workers of various types, including direct care workers, nurses, physicians and the healthcare workforce at large. For this project, the issue of energy resilience as it relates to healthcare facilities was researched and discussed with states, as this is an ongoing issue for hospitals and direct care facilities, especially during times of extreme stress such as heat waves and disasters.

The NGA Center hosted a roundtable for state and territorial leaders and private partners in December 2022 to discuss emerging topics related to energy resilience for healthcare facilities. Drawing upon recommendations and guidance from the 2019 Federal Emergency Management Agency (FEMA) and U.S. Department of Health and Human Services (HHS) report “Healthcare Facilities and Power Outages,” the NGA Center developed the roundtable to facilitate specific discussion on the best possible actions Governors and states can take to position healthcare facilities for energy stressor events and foster energy resilience for healthcare facilities.
Two NGA Center teams, the healthcare delivery and energy teams, worked collaboratively to invite a range of stakeholders to the table to foster better understanding about what role state and territorial leaders could have in supporting possible improvements to support various types of healthcare facilities and their patients. Bringing the expertise of these two NGA Center teams provided the opportunity to bring voices from both the healthcare and energy industries to support this effort. The roundtable included state and territorial policy makers, federal government agencies, healthcare organizations and energy industry experts.
Background
Healthcare facilities across the country are dependent on an adequate supply of power for the provision of both patient care and critical systems support. Across the United States, there are a wide range of healthcare facilities with a portion (approximately 17 provider types) falling under both state and federal regulations for emergency preparedness (FEMA 2019). The rest of the range of healthcare facilities (e.g., assisted living facilities, people receiving in-home care) are not regulated by Centers for Medicare and Medicaid Services (CMS) but also provide care that is dependent on electricity (FEMA, 2019). As challenges to power supply and outages occur with nearly every major disaster, coupled with pre-existing growing concerns over grid capacity and increased demand for power-dependent technologies, it is important that there are specific plans in place to ensure healthcare providers have adequate backup power and resources to operate through a prolonged energy outage since moving patients is always a solution of last resort.
Between 2000-2021, there were at least 1,542 documented power outages in the United States attributable to weather related power outages such as winter weather and severe weather. In addition, the average annual number of weather-related power outages increased by roughly 78% from 2011 to 2021, compared to the previous decade. More alarmingly still, these statistics do not include outages caused by non-weather events such as technical problems, vandalism or intentional sabotage, which are also on the rise in the United States. These observations indicate that energy resilience, especially for healthcare facilities, will remain a key factor in local and state policy making.
The Landscape of Healthcare Facility Energy Resilience
Despite the best efforts of Governors, their staff and private sector partners, rapid restoration of energy to a healthcare facility may not be immediately possible during energy stressor events. The structure of the energy infrastructure system may make prioritized restoration of healthcare facilities difficult or even temporarily impossible.
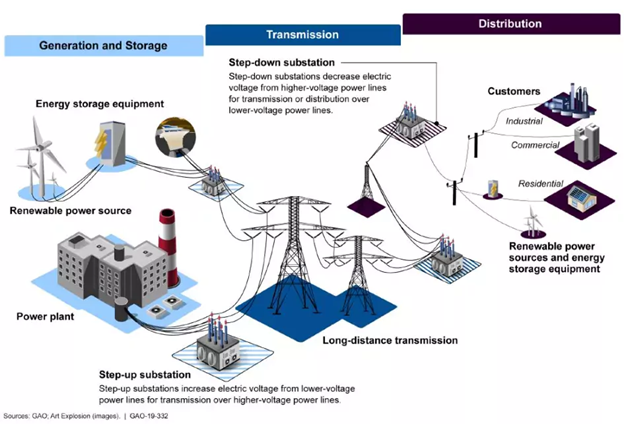
Broadly speaking, the electrical grid works in a “hub and spoke” manner. A power source, such as a power plant or wind farm, produces electricity, then high voltage transmission lines transmit this electricity across larger distances to regional substations. Finally, smaller distribution lines connect electricity to homes and businesses.
In a widespread energy disruption event, multiple substations and/or electrical lines may be damaged. As such, energy restoration along a transmission line may not be possible until each substation is repaired. Put a different way, the engineering physics of the grid may not allow for rapid restoration of energy to a healthcare facility, even if it is designated as a priority by the Governor or utility companies. The same is true of natural gas, oil and diesel distribution infrastructure. If central nodes in the system are damaged or destroyed, restoration may not be possible in a timely manner. Together, these issues mean that healthcare facilities need to be ready to become self-sufficient, at least temporarily, to continue to provide services to patients during an energy emergency.
When identifying best practices to support healthcare facility energy resilience, it is essential to identify the facilities with the highest need. These include communities and facilities more susceptible to natural disasters, rural communities with a limited number of providers, and facilities with emergency energy assurance procedures and protocols that have not kept pace with increased energy demand to support adequate services.
Backup energy systems for healthcare facilities tend to fall into two categories: 1) stored energy devices and 2) emergency generators. Stored energy devices, such as battery storage, are intended for short duration emergency power (often 90 minutes or less). These systems can allow for safe egress from a facility if evacuation is needed. More commonly, however, stored energy devices are used to bridge the gap between an initial energy interruption and the resumption of energy via emergency generators. Emergency and standby generators are designed to provide ready supplies of energy for a longer duration blackout. Generators consist of an engine, a synchronous generator, monitoring equipment and controls. Emergency generators require time to ramp up to full capacity, which necessitates the short-term use of energy storage devices discussed above.
The vast majority of emergency generators operate on fossil fuels, typically natural gas or diesel gasoline. Most emergency generator systems function well as long as they have a secure supply of fuel. This is a key point, however, because this can become a challenge during prolonged power outages. Onsight fuel storage will usually be sufficient for short- or medium-term energy disruptions. Long-term disruptions, however, lasting more than a few days, may affect the ability to restock fuel, potentially placing the facility at risk. Furthermore, relying on a single generator or single fuel source creates the possibility that a single point of failure, such as a mechanical issue in the generator or flooding and storm damage, can disable the facility’s emergency power.

Earlier this year, CMS clarified through a categorical waiver that a Health Care Microgrid System (HCMS) can be substituted in place of traditional emergency generation in many healthcare facilities. While HCMSs can be substituted in place of traditional generation, healthcare facilities that already operate backup generation could use this clarification to layer HCMSs onto their existing systems. This would eliminate the “single point of failure” issue and bolster resilience in critical healthcare functions. It is important to note that the waiver “excludes long-term care facilities that provide life support because 42 CFR 483.90(c)(2) requires these facilities to have an emergency generator without exception.”
Reliance on stored energy devices and emergency energy generation in an energy emergency lasting more than a few days can create problems that are marginal at first but escalate over time. Since emergency energy generation often cannot cover all healthcare facility operations, less critical systems may be reduced or turned off completely. A healthcare facility could endure the loss of important, though not critical systems, such as laundry services, in the short term. The loss of other systems such as water/wastewater, patient monitoring technology and communications, and HVAC/climate control are critical and present risks to patients immediately after an outage. If an energy outage stretches into days, the loss of these systems can mount, potentially jeopardizing the health and hygiene of the whole facility and the lives of the patients they are serving. Long duration energy outages could also include damage to the infrastructure needed to continue emergency backup generation. For example, major damage to roadways could prevent contractors from resupplying natural gas or diesel fuel needed to support emergency generation at healthcare facilities. Worse still, healthcare facilities in the immediate area might rely on the same contractor(s) to provide resupply services. Damage to the contractor equipment, disruption to contractor labor force or even emissions regulations if not waived could prevent restocking of fuel across multiple healthcare facilities in the region.
It is also important to consider the intersection of challenges between emergency planning and staffing due to healthcare workforce challenges. The healthcare workforce has seen significant shortages, further exacerbated by the COVID-19 pandemic, over the past few years. During an energy emergency, an increased burden is placed on larger or more developed facilities such as community hospitals and major trauma centers with emergency power supply, including an influx of patients coming from other facilities, coupled with existing staffing shortages. During a disaster or other energy emergency that cannot be remedied quickly, the emergency plan for smaller facilities is to evacuate patients to larger hospitals as a last resort. Additionally, in the event of an evacuation due to an energy emergency, staffing shortages or lack of training on emergency preparedness could create additional barriers for service delivery among healthcare facilities leading to additional health complications and potential detriments leading up to loss of lives.
Recommendations for State and Territorial Leaders
Below are some best practices that the NGA Center gathered from the roundtable experts’ discussion that could support state and territorial leaders in providing opportunities that best position healthcare facilities when energy stressor events occur, prioritizing healthcare facility energy resilience.
- Emergency Communication Plans: Establishing communication plans between state and local governments, utilities and healthcare facilities can help ensure appropriate prioritization for high-risk facilities
- Critical System Planning: Backup generation may not be sufficient to meet all energy needs for healthcare facilities. As such, difficult decisions on which critical systems should be prioritized may need to be considered before an energy stressor event occurs and exacerbates existing challenges. Although CMS and state regulations require on-site backup generation, practices for fuel storage, scheduled maintenance and technical staff to maintain and repair systems, vary widely across healthcare facilities.
- Coordinating Exercises: States can include the healthcare sector in emergency response exercises, including energy emergency exercises.
- Evaluating Vulnerabilities Governors and their staff can carefully study energy system vulnerabilities and potential restoration delays to energy restoration to pre-plan needed support to those facilities that are most vulnerable and most likely to suffer a longer duration outage.
- Engaging Utilities: It is critical that state and territorial leaders, healthcare facilities, healthcare providers of all training levels and utilities are engaged in planning for energy assurance to ensure the best energy resilience for healthcare facilities. Such partnerships would allow healthcare facilities and utilities to explore jointly energy systems, such as microgrids, that might otherwise be cost prohibitive.
- Leveraging Funding: Additional funding for modernizing healthcare facility energy infrastructure coupled with technical assistance for states during this process would enable facilities to bolster and expand their existing emergency generation and energy storage systems without facing steep upfront costs. Many states and municipalities also offer innovative financing for energy efficiency programs. Programs like Commercial Property Assessed Clean Energy (C-PACE) allow healthcare facilities to use borrowed capital to pay for the upfront costs associated with energy efficiency or renewable energy improvements. Unlike other project financing, the borrowed capital is repaid over time via a voluntary tax assessment. Substantial federal funding for grid resilience has been allocated by Congress in the Infrastructure Investment and Jobs Act (IIJA) and the Inflation Reduction Act. Several key provisions of these pieces of legislation could be leveraged by state and local policy makers and healthcare facilities to strengthen resilience, including federal dollars to support the healthcare workforce, in efforts to prioritize energy resilience (e.g., American Rescue Plan Act funding).
- Engaging Healthcare Facilities in Planning: Governors can incorporate healthcare facilities and their specific needs to maintain care provision at a range of facility types into state energy security plans and emergency response exercises. These facilities could include direct care facilities such as; nursing homes, skilled nursing facilities, and rehab hospitals, inpatient and outpatient mental health and substance use treatment facilities; and supports for in-home care providers.
- Preparing for Worst-Case Scenarios: Planning and preparation are required to modernize emergency infrastructure in healthcare facilities. Such planning can positively affect service delivery in the event of an energy emergency. Three days without power, in what has been termed a “black sky event,” can have cascading effects for healthcare facilities and could lead to a facility being evacuated for a non-energy related issue (e.g., water, wastewater, climate control) that is essential for the provision of care. According to the FEMA/HHS report used to inform this project, evacuation and relocation of patients in healthcare facilities is never a best practice and should be avoided if possible as it may lead to destabilizing patients, injuries, other new health concerns and poorer overall health outcomes. Improving facility preparations and infrastructure improvements can help provide supportive care environments in the event of prolonged outages.
Conclusion
The NGA Center was able to take recommendations and best practices shared during this roundtable to assist in project planning for the future and will continue to bring together state and territorial leaders to engage in peer learning and information sharing. In addition, this brief may be helpful for Governors and states engaged in comprehensive infrastructure planning as they are considering ongoing improvements to larger systems and planning policies.
Acknowledgements
The National Governors Association Center for Best Practices would like to thank the Health Resources and Services Administration (HRSA) in the U.S. Department of Health and Human Services for their generous support in the development of this publication under National Forum Cooperative Agreement No. U98OA09028. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of HRSA or the U.S. Department of Health and Human Services.
The NGA Center would like to thank the state officials and subject matter experts whose expertise contributed to this publication as well as the NGA, HRSA and Department of Energy staff who contributed expertise and review of this publication.
Citation
McCabe, E., Fletcher, C., Hockenberry, S., Lauf, D. Prioritizing Resilience: Recommendations for State and Territorial Leaders on Energy Resilience for Healthcare Facilities. Washington, DC: National Governors Association, April 2023.
Resources for States
- Addressing Wages of the Direct Care Workforce Through Medicaid Policies
- Axios: Attacks on Power Grid Raise Alarm Among Top Officials
- Department of Energy: C-PACE Fact Sheet
- Healthcare Facilities and Power Outages
- IIJA Implementation Resources
- Inflation Reduction Act: Infrastructure Implementation Resources
- NGA Healthcare Workforce Page
- State Strategies For Sector Growth And Retention Of The Direct Care Health Workforce
- Climate Central: Surging Weather-related Power Outages