This publication explores strategies Governors and state leaders employed to address the longstanding issues associated with behavioral health among the maternal and child health (MCH) population.
(Download)
This is the fourth in a series of five publications focused on COVID-19’s impact on maternal and child health (MCH) programs and populations in the U.S. Each publication focuses on a facet of MCH, including COVID-19 response and recovery, health and human services workforce, childcare, behavioral health, and community supports. The information contained in this series comes from a culmination of interviews and research conducted between early 2022 and January 2024, including an expert roundtable held in the Summer of 2022.
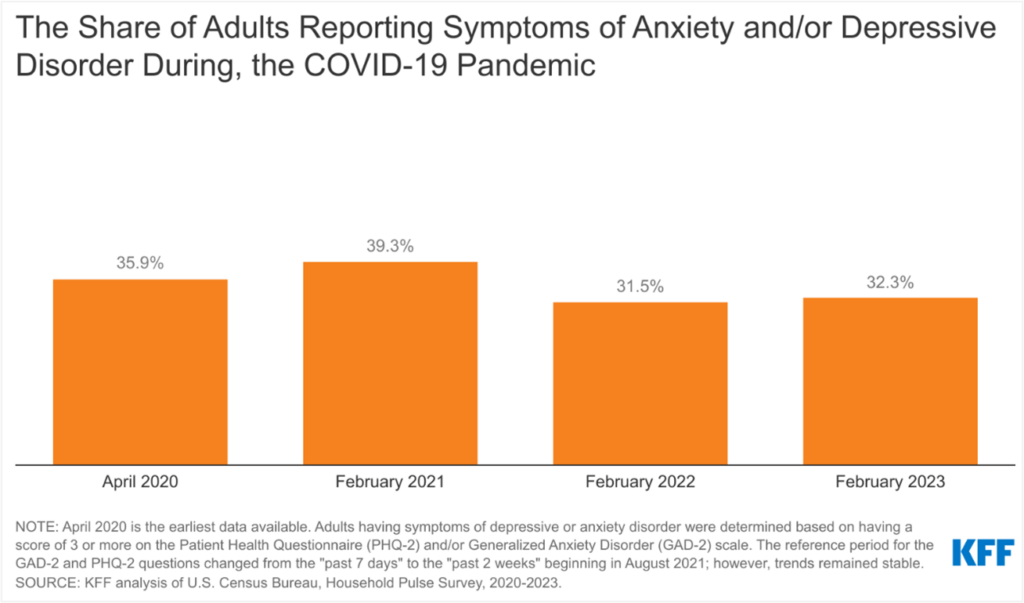
The COVID-19 pandemic spurred a significant decline in many Americans’ mental health, felt especially among children, adolescents – specifically teenage girls – and women., Substance use or misuse is often a coping mechanism for individuals suffering from an untreated or undiagnosed mental health condition, making the two inextricably linked. Untreated mental health conditions can have negative effects on a person’s wellbeing and physical health, which are further exacerbated by substance use, especially at critical development stages. For example, untreated, sustained stress among pregnant people can lead to high blood pressure and heart disease – both are linked to maternal and infant mortality and morbidity. In addition, people using substances during pregnancy may delay or avoid prenatal care altogether due to fear of stigma and legal consequences, which can contribute to adverse health outcomes. Untreated mental health conditions can also be expensive for individuals and insurance payers. In 2017, the estimated societal cost of untreated perinatal mood and anxiety disorders in the U.S. equated to $14.2 billion – about $32,000 per mother-child pair.
COVID-19 mitigation measures such as quarantine, social distancing, school and child care closures, grief after bereavement, financial worries, fear of infection, and major disruptions in mental health services resulted in diminished mental health and increased substance use. The U.S. saw an increase in substance and alcohol use during peak lockdown months, as well as shifts in the illicit drug supply. During the first year of the pandemic, suicide and overdose became significant contributors to pregnancy-related maternal deaths. Depression, anxiety, and stress also rose among those aged 4 to 19. Although the pandemic exacerbated mental health conditions and substance misuse, these challenges predated the pandemic. Youth were experiencing increased major depressive episodes in 2019, while access to mental health providers was limited. The use of mental health-related emergency services rose by 42 percent between 2016-2019, and drug overdose deaths rose by 21 percent between 2015 and 2016. Three years after the COVID-19 lockdowns, the U.S. is facing an even steeper uptick in those seeking treatment for mental health and substance use disorder. Governors and state leaders can address behavioral health by increasing access to and resources for mental health services and supporting initiatives to prevent maternal and adolescent substance use. State partnerships with private industry, hospital systems and community health organizations can address disparities and improve perinatal health outcomes.
Governors’ Strategies
This publication explores strategies Governors and state leaders employed to address the longstanding issues associated with behavioral health among the maternal and child health (MCH) population. Some of these efforts include:
- Improving access to mental health services for pregnant and parenting women, parents and families.
- Addressing the mental health crisis among children and adolescents by offering wider access to prevention and treatment services.
- Supporting initiatives to prevent maternal substance use disorder, substance misuse and tobacco use.
- Exploring options to provide broad access to tele-behavioral health services, especially for disproportionately affected populations and in areas with limited in-person service options.
Improving Access to Mental Health Services for Pregnant Women, Parents and Families
Maternal mental health conditions affect as many as 800,000 families annually. In 2021, more than one in five women experienced a mental health condition. Stigma and misunderstanding prevail as primary barriers to access outside of cost, coverage, provider capacity and other logistical limitations. Although postpartum depression is one of the most well-known pregnancy-related mental health conditions, current and recently pregnant people may experience new or relapsed anxiety, post-traumatic stress disorder, obsessive compulsive disorder, mania, psychosis and/or dysthymia. For women, anxiety and depression alongside substance use or misuse are the most common co-occurring diagnoses.
Despite having a higher interaction with providers during the prenatal period, only about 15 percent of women diagnosed with a maternal mental health condition receive treatment. Suicide is also a leading cause of death for women while pregnant through the first year postpartum. The Colorado Department of Public Health and Environment launched a campaign to encourage mental health discussion with providers alongside a program to reduce mortality. The program developed resources for clinicians to identify, treat and refer pregnant women experiencing mental health challenges. A survey of recently pregnant women who attempted suicide or overdosed, as well as their close family, friends and providers informed the resources. New York state developed a Perinatal Mood and Anxiety Disorder State-wide Resource Directory to improve access to behavioral health resources. The directory includes contact details and information on mental health services broken down by categories such as providers accepting Medicaid, bilingual and multi-lingual providers, support groups, telehealth and more. Additionally, the Legislative Analysis and Public Policy Association released a model law on how states can appropriately address substance use during pregnancy in 2023.
In addition to the strategies outlined above, Governors may also consider:
- Providing materials and resources to the public on pregnancy-related depression and anxiety and postpartum depression and anxiety.
- Encouraging pregnant and postpartum women to discuss mental health with their providers.
- Working with hospital systems to offer coping skills and support resources to pregnant women and new mothers.
- Implementing the 988 National Suicide Prevention Lifeline or other mental health crisis line to connect individuals in crisis with appropriate personnel.
- Working with the state’s Medicaid agency to require maternal depression screening in well-child visits.
- Increasing access to overdose education and Naloxone distribution.
- Leveraging resources to implement harm reduction strategies for pregnant people with substance use disorder, such as the Harm Reduction Coalition’s Pregnancy and Substance Use Toolkit.
- Promoting awareness and use of 1-833-TLC-MAMA [1-833-852-6262], the National Maternal Mental Health Hotline, to connect pregnant and postpartum individuals that need 24/7 emotional support, resources and referrals.
- Supporting health care organization and clinician awareness and sharing of the National Maternal Mental Health Hotline Partner Toolkit through all communication forms in-person, social media and print to connect individuals to hotline services.
- Expanding training and support for peer-support model implementation with group interventions focusing on behavioral and physical health and wellness during pregnancy, birth and early parenthood with flexibilities for in-person and remote (on-line, teleconference, and telephone).
Addressing the Mental Health Crisis Among Children and Adolescents
In the decade before the pandemic, suicide rates among youth aged 10-24 increased by 57 percent. According to the CDC’s annual Youth Risk Behavior Survey, more than 40 percent of students experienced persistent feelings of sadness or hopelessness in 2021 – a 5 percent increase from the year prior. Additionally, one in five students reported “seriously considering attempting suicide” in 2021 – a 3 percent increase from 2019. Female students and Black students had the highest rates of suicidal ideation.
Intervention and connection to treatment are most critical during childhood and adolescence for youth with mental health conditions. More than half of all mental disorders emerge before a person turns 14 while 75 percent of disorders emerge before a person turns 24. The most common disorders among children aged 3-17 are attention-deficit/hyperactivity disorder (ADHD) and anxiety, followed by behavior problems, and depression. Compounding the increase in mental health concerns, youth and families struggle to find and obtain quality, affordable mental health care. Only 20 percent of children with a diagnosable disorder receive care from a specialized provider. In March of 2022, Utah Governor Spencer Cox signed S.B. 171 to develop a mental health curriculum for elementary and secondary public schools. The curriculum aims to raise awareness, build resiliency in students and take an upstream approach to preventing mental health disorders. In January of 2023, Minnesota Governor Tim Walz released a supplemental budget allocating nearly $10 million dollars to enhance school-based mental health screening and $3.7 million to expand access to infant and early childhood mental health programs.
In addition to the strategies outlined above, Governors may also consider:
- Providing Medicaid reimbursement for infant, early childhood, school-based, and community-based mental health services in all early childhood settings, such as pediatric care, child care, and home visiting.
- Compelling state agencies that regulate public and commercial insurance systems to enforce parity standards between coverage for mental and physical health.
- Developing legislation to support access to mental health services for students through school-based mental health services.
- Allowing for COVID-related flexibilities around telehealth reimbursement to continue after the unwinding of the public health emergency.
- Working with departments of education and school systems to provide training to teachers and school administrators to address mental and behavioral health.
- Ensuring that districts have substance use prevention programs and access to naloxone to respond quickly to overdose.
STATE ACTIONS
The Colorado Behavioral Health Administration (BHA) launched the I Matter Program in 2021. The program provides youth 18 and younger with six free, confidential therapy sessions with a licensed provider. The I Matter program is funded through the American Rescue Plan Act and has served more than 2,600 youth since its implantation. Although in-person support is available, most appointments are virtual through a partnership with Mindhues.
Supporting Initiatives to Reduce and Prevent Maternal Substance Use
Alongside suicide, substance overdose – whether intentional or unintentional – is one of the leading causes of death for women in the perinatal period. Many women with a substance use disorder (SUD) also have a history of trauma, often perpetrated by a trusted person. Women with opioid use disorder (OUD) report high rates of intimate partner violence, which persists as a cycle either because substance use is a coping mechanism for the violence or the violence prohibits access to proper recovery. Services for those with SUD must have a trauma-informed approach to address painful experiences people who use drugs may be coping with or trying to escape.
Stigma associated with substance use is pervasive regardless of the individual or circumstances, however, it is especially so for pregnant women. Pregnant women with SUD face judgment and negative interactions with providers, affecting their willingness to divulge their condition and connect to treatment. Some state programs provide pregnant women with SUD a plan of safe care (POSC), which is a tool to address negative effects of substance use in newborns, but also keeps mothers with their infants and connects them to treatment. In Tennessee, the Ridgeview Behavioral Health Center created the Mothers and Infants Sober Together (MIST) program to work with parents seeking treatment. The program, embedded in the state’s health care system, state agencies, and county departments, obtains referrals and links patients to treatment and recovery services.
In addition to the strategies outlined above, Governors may also consider:
- Creating partnerships between state agencies responsible for MCH and behavioral health services to streamline supports for pregnant and postpartum women with a behavioral health condition such as substance use disorder.
- Establishing a committee, task force or other group to determine policies and programs that would improve maternal health and address substance use disorder and include relevant state staff, people with lived experience, community leaders and providers.
- Increasing pathways for training and increase workforce of community health workers (CHWs) and peer-support specialists to include individuals with lived experience of maternal SUD, OUD and IPV.
- Bolstering training, certification and workforce of state recognized CHWs to engage pregnant and postpartum women to identify SUD, OUD, and IPV and provide direct access to education and treatment.
STATE ACTIONS
The West Virginia Drug Free Moms and Babies Project (DFMB) began as a pilot in 2011 – funded through the Claude Worthington Benedum Foundation. DFMB grew in 2021 through Substance Abuse and Mental Health Services Administration (SAMHSA) funding. DFMB is a collaborative effort across state departments and offices with sites in 16 counties. Under this program, the mother is partnered with a care coordinator to link her to wraparound services, including SUD treatment, home visiting, housing, peer recovery coaches and more. The number of women who initially test positive for a substance upon enrollment decreases by 40 percent by delivery, and 74 percent of infants are discharged from the program with their mothers.
The Oklahoma State Department of Health worked with the University of Oklahoma to establish and expand STAR (Substance Use Treatment and Recovery) Prenatal Clinic tailored to the needs of women with a history of substance use. Eighty-four percent of infants were discharged home in the custody of their biological parents through the program. Additionally, Oklahoma instituted TeamBirth, a process to improve clinical safety effective communication, and dignity in childbirth through labor huddles centered around mothers in 34 of Oklahoma’s 44 birthing hospitals. Results were improved trust and autonomy scores from Oklahoma mothers across races and ethnicities.
Exploring Options to Provide Broad Access to Tele-Behavioral Health Services
Telehealth utilization increased dramatically during the COVID-19 pandemic, representing about 13 percent of outpatient visits in March and April 2020. Since then, telehealth use has plateaued at 36 percent — just under pandemic levels for mental health and SUD treatment. Pandemic flexibilities in reimbursements and provider licensure have remained with the federal public health emergency; however, its ending in May 2023 affected how some states allow telehealth services to operate – depending on changes the state has made in since 2020. For example, 21 states have implemented payment parity and six states have parity with caveats so providers will be reimbursed at the same rate as an in-person visit.
Additional telehealth access challenges persist, such as providers working across states lines and limited broadband access in certain areas. In 2023, Wyoming Governor Mark Gordon signed S.B. 26, allowing psychologists to practice telepsychology across state lines. In 2019, former Louisiana Governor John Bel Edwards lunched a Broadband for Everyone Louisiana Commission via executive order to close the digital divide in the state within ten years. The Commission was a catalyst for a 2022 program, Granting Unserved Municipalities Broadband Opportunities (GUMBO), allocating American Rescue Plan funding to 77 programs to improve broadband access in over 50 parishes.
In addition to the strategies outlined above, Governors may also consider:
- Providing greater access to technology to provide telehealth services including clinical, home visiting, mental health and social services to greater populations.
- Improving broadband access to rural and under resourced areas of the state.
- Allowing telephone or “telephonic visits” to qualify as a telehealth visit and be reimbursable as such.
- Waiving the need for a pre-existing patient-provider relationship to access a provider through telehealth or receive e-prescribing of medications.
- Limiting cost-sharing for patients for telehealth visits.
- Encouraging widespread training for any provider able to see patients via telehealth to ensure the workforce can meet patient needs appropriately.
- Evaluating cross-border licensing issues for telehealth Medicaid reimbursement by collaborating with state licensing boards and Medicaid agencies to determine a path forward.
Conclusion
Behavioral health is a longstanding issue for Americans, and the COVID-19 pandemic has worsened and highlighted the gaps in the delivery of behavioral health services. Establishing systems to improve not only access to care, but access to quality care that is trauma-informed and affordable is critical. Governors have a variety of options to establish policy pathways for treatment and care within the behavioral health space with many already spearheading efforts to make progress in this area.
Acknowledgments
The NGA Center would like to thank the state officials and experts who participated in the June 2022 expert roundtable as well as those who provided feedback to inform this publication. The NGA Center would also like to thank the Health Resources and Services Administration in the U.S. Department of Health and Human Services for their generous support of this project. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of HRSA or the U.S. Department of Health and Human Services.
This publication was developed by Michelle LeBlanc, Jessica Kircher, Asia Riviere, and Brittney Roy at the National Governors Association Center for Best Practices.
Recommended citation: LeBlanc, M., Kirchner, J., Riviere, A., & Roy, B. (2024). State Strategies to Address the Impact of COVID-19 on Maternal and Child Populations: Maternal & Child Behavioral Health. Washington, D.C.: National Governors Association Center for Best Practices.