This paper looks at comprehensive local and state programs that can assist people with diabetes who may have low-incomes, be older or live in underserved communities.
(Download)
Type 2 diabetes, a preventable condition where a person’s body cannot regulate blood sugar properly, has a staggering impact on the health of many in the United States. Of the 37.3 million U.S. adults with a type of diabetes, 90-95% have type 2 diabetes. Additionally, 96 million American adults have prediabetes where their blood sugar is higher than normal. It is estimated that 23% of U.S. adults with diabetes do not know that they have diabetes, and 8 in 10 U.S adults do not know they have prediabetes. Diabetes can lead to complications including kidney-failure, lower limb amputation, adult blindness, gum disease and tooth loss and is the seventh leading cause of death.
The estimated total economic cost of diagnosed diabetes is $327 billion, including healthcare costs and loss of productivity, with $1 out of $4 U.S. health care dollars spent on caring for people with diabetes. On average, people with diagnosed diabetes have medical expenditures that are approximately 2.3 times higher than what expenditures would be in the absence of diabetes.
Diabetes can develop from a combination of genetic and environmental factors, including family history, a sedentary lifestyle and unhealthy eating habits. Social determinants of health, including income, education, housing and access to healthy foods contribute to the development and progression of type 2 diabetes. Diabetes disproportionately impacts racial and ethnic minority populations, and despite their higher prevalence of diabetes, they are less likely to receive recommended diabetes preventive care and treatment.
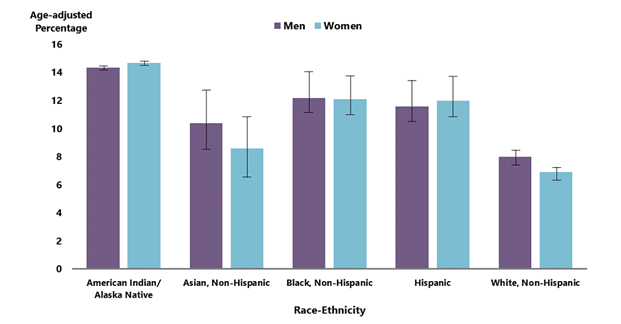
For both men and women, prevalence of diagnosed diabetes was highest among American Indian and Alaska Native people (14.5%) and non-Hispanic Black people (12.1%), followed by people of Hispanic origin (11.8%), non-Hispanic Asian people (9.5%) and non-Hispanic White people (7.4%) in 2018-2019.
In January 2022, the National Governors Association Center for Best Practices (NGA Center) launched the Strategies for Preventing and Managing Type 2 Diabetes Learning Lab (Diabetes Learning Lab). The purpose of the Diabetes Learning Lab was to support Governors and state officials as they work to improve population health, reduce health care spending and reverse negative health trends by investing in comprehensive state plans to prevent or delay type 2 diabetes. Over the six-month period, Governor-appointed representatives from four states: Maryland, Alabama, Alaska and Delaware participated. During the learning lab, Maryland was featured as an innovator state and shared best practices and lessons learned with the other three states. The participants convened in virtual workshops covering a wide range of topics related to the following:
Learning Lab 1: The National Diabetes Prevention Program (National DPP) Lifestyle Change Program
Learning Lab 2: Food Security and the Built Environment
Learning Lab 3: Telehealth and the Healthcare System
Learning Lab 4: Diabetes Self-Management Education and Support (DSMES) Services and Medication
As a part of the Diabetes Learning Lab, states discussed themes and policies for type 2 diabetes prevention and management in three buckets: primary, secondary and tertiary prevention. Through research and discussions prompted by states during the learning lab, the NGA Center developed a framework to guide how state leaders can address type 2 diabetes prevention and management in their state. The framework created appears in Figure 1.
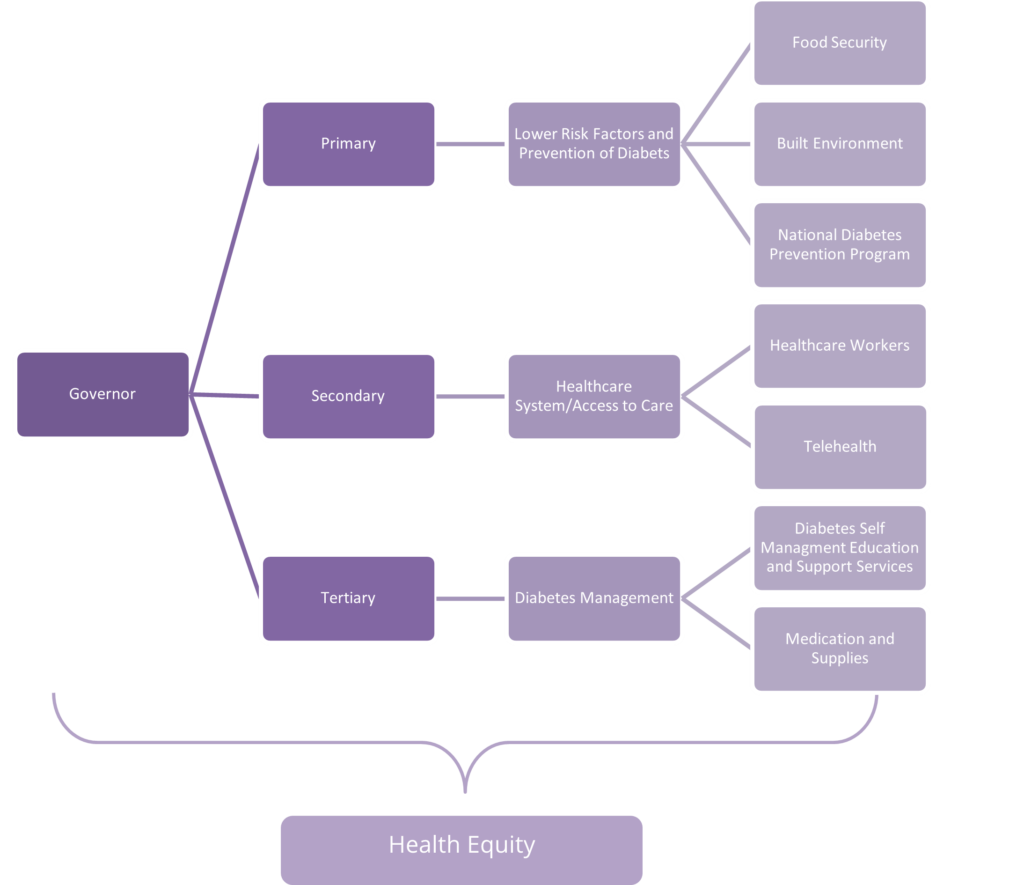
This action plan includes considerations discussed during the learning lab and associated research. First, the paper highlights policies that states can use to lower risk factors that contribute to type 2 diabetes diagnoses and promote lifestyle changes. Next, the paper identifies strategies to reduce the impact of diabetes through early detection and robust access to care. Lastly, the paper identifies considerations to help people manage diabetes and prevent diabetes-related complications. Governors can use this publication as an action plan to reduce the burden of diabetes in their state.
Considerations for Governors
Primary prevention – Prevent or delay type 2 diabetes by lowering risk factors and promoting lifestyle changes
- Consideration One: Create and support state-level policy that expands coverage of the National Diabetes Prevention Program
- Consideration Two: Implement policies to increase enrollment and retention in the National Diabetes Prevention Program
- Consideration Three: Expand access to nutritious foods
- Consideration Four: Increase neighborhood and physical environment walkability
Secondary Prevention – Reduce the impact of diabetes through early detection and access to care
- Consideration Five: Use telehealth to help address disparities in diabetes management outcomes
- Consideration Six: Use non-traditional health care providers and practices to create more sustainable and overarching means of care
Tertiary prevention – Help manage diabetes and prevent diabetes-related complications
- Consideration Seven: Increase referrals to diabetes self-management education and support services
- Consideration Eight: Increase pricing transparency to lower the cost of diabetes care
Type 2 Diabetes is a chronic health condition that affects how the body turns food into energy.
Most of the food people eat is broken down into sugar and released into your bloodstream. When a person’s blood sugar goes up, it signals the pancreas to release insulin. Insulin acts like a key to let the blood sugar into the body’s cells for use as energy.
If someone has diabetes, their body either doesn’t make enough insulin or can’t use the insulin it makes as well as it should. When there isn’t enough insulin or cells stop responding to insulin, too much blood sugar stays in the bloodstream.
Learning Lab 1: National Diabetes Prevention Program
During the 2022 Learning Lab, states first discussed the National Diabetes Prevention Program (National DPP), a lifestyle change program created by the Centers for Disease Control and Prevention (CDC). The participants discussed their states’ varying amount of Medicaid coverage and how to increase accessibility to the National DPP through referrals and recruitment.
Consideration One: Create and support state level policy for coverage of the National Diabetes Prevention Program.
The National DPP lifestyle change program is an affordable, high-quality program proven to help people prevent or delay type 2 diabetes. Through helping people with prediabetes learn about healthy eating habits, exercise and stress relief participation in the National DPP can lead to weight loss and cut the risk of developing type 2 diabetes by 58% (71% for people over 60 years old). CDC sets standards for organizations that wish to offer a lifestyle change program. To achieve CDC recognition, organizations must show that they are following a CDC-approved curriculum and achieving meaningful results with patients based on established national standards.
How do you prevent diabetes?
- Lose 5-7% of body weight
- Get 30 minutes of physical activity 5 days per week
- Eat smaller portions and healthy foods most of the time
- Avoid smoking
- Minimize alcohol consumption
Governors can utilize their executive power to support increased insurance coverage for the National DPP. One way this can be done is by championing Medicaid coverage. Medicaid recipients are more likely to have prediabetes and be hospitalized for diabetes-related issues such as kidney disease, lower limb amputation and heart and vascular issues compared to the average U.S. population. State Medicaid coverage for the National DPP can connect Medicaid-eligible populations to a framework to reduce their risk of type 2 diabetes and improve their overall health. Barriers to implementing Medicaid coverage include lack of Medicaid payer support, limited communications between state agencies and difficulty gathering data for the National DPP.
Through the Diabetes Learning Lab, states and subject matter experts discussed potential solutions that states can implement to overcome these challenges.
Create state initiatives for Medicaid coverage of the National DPP
As of 2022, 20 states have Medicaid coverage for the National DPP. Governors can use their executive authority and encourage stakeholders to bridge the gap and provide pathways for preventative care. By collaborating with the state’s legislature, state Medicaid department and health department, Governors can work to achieve National DPP coverage for low-income populations in their state who are eligible for Medicaid. Nationally, Medicaid covers one in four individuals, which makes Medicaid a key lever to drive population health improvement. States have achieved Medicaid coverage for the National DPP through the following pathways:
- State Plan Amendment (SPA): States submit amendments to alter a state rule or policy within the current Medicaid law and regulation. States must receive approval from the Centers for Medicare and Medicaid Services (CMS) to make such changes to their state plan. Certain requirements, like offering the benefit statewide, apply when using the state plan pathway.
- Section 1115 Waiver: If the state wants to create a more narrow pilot program or test an approach that otherwise wouldn’t be allowed under the state plan, the Medicaid program can submit an 1115 waiver. The 1115 waiver, if approved by CMS, would allow the state to create a pilot program for coverage and is often used for a new program deemed more experimental for states determined eligible. It is important to keep in mind that additional requirements and reporting burden are associated with 1115 waivers, and these waivers are also subject to CMS review and approval.
Use pilot programs to create the case for state coverage of the National DPP
Over the course of the Diabetes Learning Lab, states and subject matter experts discussed working with managed care organizations (MCOs) as a means to create a pathway for Medicaid coverage of the National DPP. States that use a managed care model can encourage or contractually require MCOs to offer the National DPP lifestyle change program to the subset of the Medicaid population that receives care from that MCO. One way this can be done is through MCO pilot programs, where a state can contract with a single MCO or multiple MCOs in offering the program to a subset of its members. Pilot programs can help the state determine the effectiveness of the National DPP for certain populations, whether there are sufficient National DPP organizations in the state and the fiscal impacts on MCOs and state budgets. For example, Illinois launched a pilot program that contracted community-based organizations (CBOs) that are normally not reimbursed for this service to offer the National DPP with Medicaid MCOs. The success of this program led Illinois to use a state plan amendment to create National DPP as a statewide benefit for Medicaid recipients.
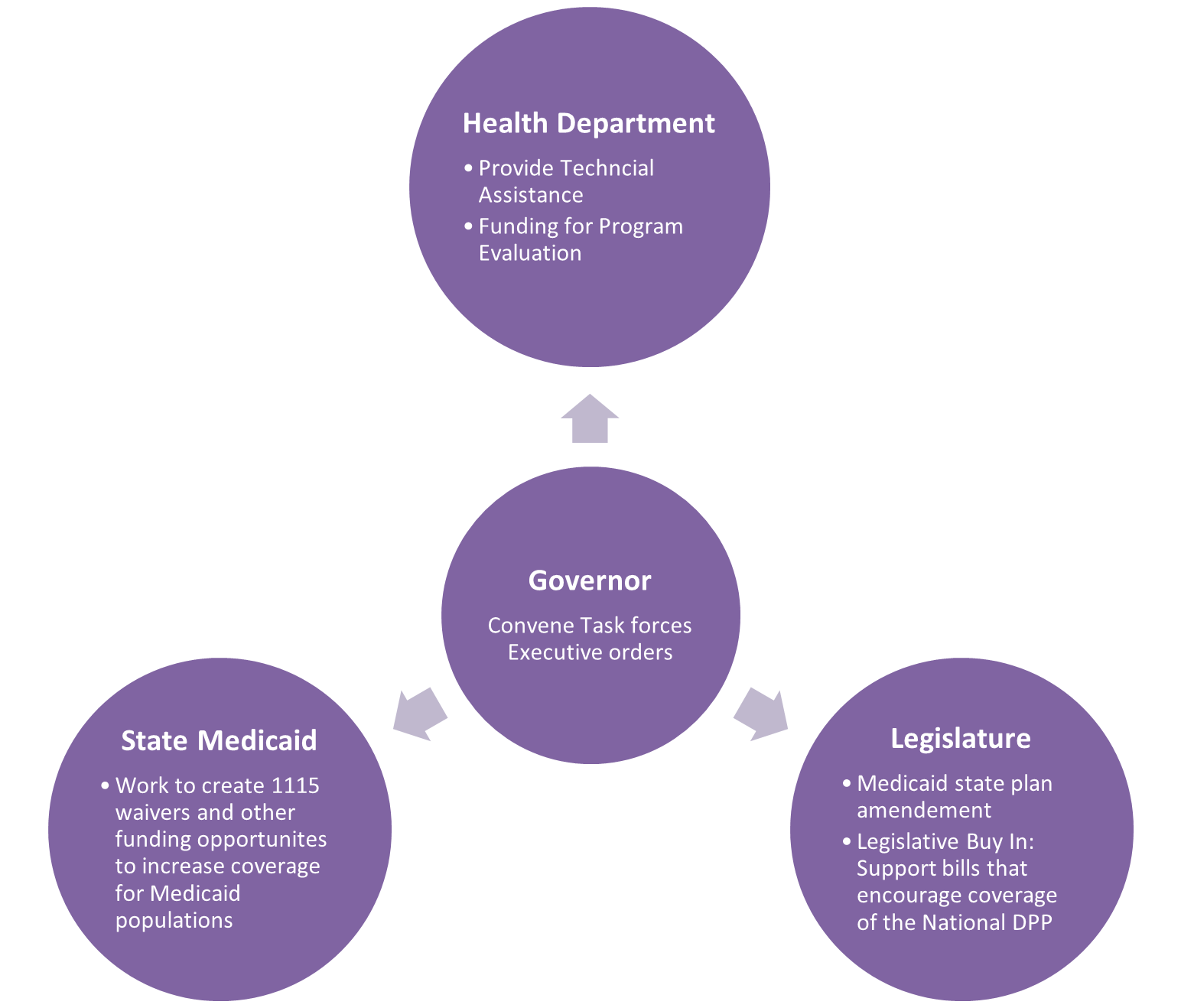
Build relationships between state agencies
Governors can create task forces or committees that include the state’s chronic disease division/department, the state’s Medicaid agency, the state legislature, relevant CBOs and health care practitioners to support the National DPP in their states. By creating taskforces or committees, supporting legislation that promotes diabetes prevention efforts and/or allocating funding in the state budget, Governors can champion and support the National DPP for Medicaid recipients. Figure 2 shows how the Governor can forge partnerships and breakdown silos in diabetes prevention.
Consideration Two: Implement policies to increase enrollment and retention in the National Diabetes Prevention Program
Even when type 2 diabetes prevention is covered by insurance, the National DPP lifestyle change program is only effective when people are aware of the program. Once coverage mechanisms are established, recruitment, referral and retention may remain difficult. A 2018 study found that only 4.2% of eligible individuals reported being referred to the program, although 25% of eligible individuals were interested. Governors may help increase recruitment to the National DPP by encouraging providers to refer patients to the program and to spread the word through the health department’s communication efforts. States have opportunities to strengthen their referral and recruitment practices, encourage the use of technology, expand the use of National DPP and reduce the burden of diabetes.
Engage health care providers in the National Diabetes Prevention Program
Individuals are much more likely to enroll in the National DPP lifestyle change program when referred by their healthcare provider. However, few providers are aware of the program or the evidence-based success behind it. To overcome this gap in awareness, Governors can share information with providers on the benefits of the National DPP and identify strategies that connect providers with organizations such as member associations. For example, Oregon improved provider awareness through a partnership with The Oregon Health Authority and the Oregon Medical Association. The two entities created a campaign called Steering Toward Health aimed at reducing the incidence of type 2 diabetes and other chronic conditions. The campaign includes a toolkit of resources designed to help providers talk to their patients about prediabetes and refer eligible patients to CDC-recognized organizations. Creating resources can help providers assess patients who will benefit from the program and help reduce the burden of prediabetes and type 2 diabetes statewide.
Develop bi-directional referral systems
Outdated referral systems and inefficient processes can contribute to recruitment and referral challenges. By streamlining the referral process, providers can have more accessible means to refer patients to the National DPP. One way this can be done is through a bi-directional referral system. Bi-directional referral systems consider both the information going from the healthcare system to the referred community program or resource, in this case a National DPP program, as well as the information going back to the healthcare system from the National DPP delivery organization. This system allows providers to maintain awareness of their patient’s status in the National DPP and to witness the effectiveness of the program firsthand. Governors can support funding for bi-directional referral systems to modernize public health data systems and increase the linkage of National DPP to people with prediabetes.
Develop marketing strategies that prioritize specific populations
Messaging about the National DPP may not reach people who are at an increased or higher risk for type 2 diabetes, including rural populations, people with disabilities, and racial and ethnic minority communities. Governors can work with interested partners to develop a variety of strategies that prioritize populations that are disproportionately impacted by diabetes. Some strategies that have found success include: word-of-mouth marketing, digital strategies and engaging providers as promotion partners. For example, word-of-mouth marketing can be especially beneficial in rural populations because of the close-knit nature of the community. In the learning lab, Delaware shared marketing efforts to target National DPP referrals to Black and Hispanic males due to higher rates of prediabetes, diabetes,and associated comorbidities among these populations. Governors can use their inter-agency oversight to increase outreach for the National DPP to refer and recruit all eligible individuals so the program has the greatest impact possible.
Improve retention for National Diabetes Prevention Program participants
Retaining participants in the National DPP is important to preventing or delaying type 2 diabetes. Studies show the longer a person participates in the National DPP, the more likely they are to achieve the benefits from the National DPP such as weight loss. Participants may not be able to complete the program due to competing priorities, poor access to transportation, food security challenges and the lack of availability of resources such as education and childcare. Telehealth can address some of these barriers, but challenges persist. By understanding unique participant needs, using low-literacy materials, encouraging social connections, offering supplemental experiences, tailoring communications and using incentives, the National DPP can continue to serve as a safe space for those with prediabetes to learn strategies to prevent type 2 diabetes. In Minnesota, National DPP participants who received incentives to remain in the program had significantly higher attendance than participants who did not receive incentives. Though incentives cannot be covered by Medicaid, providing incentives such as a free YMCA membership at key transitions can improve retention. Governors can use a combination of strategies, such as coverage support for social determinants of health (SDOH) to increase engagement and improve retention.
Learning Lab 2: Food Security and Built Environment
States can address the health inequity within diabetes incidence and prevalence by examining the Social Determinants of Health. Incorporating interventions that address lifestyle, workplace and environment can enable change. Learning lab participants discussed how to address Social Determinants of Health through state programs addressing food security and the built environment.
Consideration 3: Expand eligibility and access to nutritious foods
An estimated 10.5% of U.S. households are food secure or having, physical and economic access to sufficient food to meet dietary needs for a productive and healthy life . According to the U.S. Census, over 12.8 million households lack access to adequate food due to insufficient income or resources. People experiencing a lack of food security due to multiple factors that often intersect with the social determinants of health, including affordable housing, racism, social isolation and lack of transportation. To address their hunger, Americans experiencing food security challenges regularly choose between going without food or eating foods that are cheaper, readily available, nutrient-poor and linked to weight gain. Constant consumption of high-calorie, sugar-rich food and drinks is a contributing factor to chronic diseases, including obesity, hypertension and diabetes. Adults experiencing food security challenges are two to three times more likely to have diabetes, even when controlling for other factors.
Many people experiencing food security challenges live in food deserts, or areas without grocery stores or supermarkets offering affordable, healthy foods within convenient traveling distance. About 39.5 million urban and rural Americans live in a food desert. In urban areas, food deserts are disproportionately located within Black communities; a 2014 study showed Black communities had fewer grocery stores compared to White communities and those of the same socioeconomic levels. People experiencing food security challenges are likely to simultaneously experience financial insecurity, causing them to choose between differing needs such as medications, housing, education or healthy food. People with prediabetes and diabetes are often caught between competing priorities of a healthy diet, affording prescribed medications and supplies, or other necessities. To address issues like these, Governors can enhance data collection to identify gaps in care, expand food supplement programs to ensure access and incentivize grocery store construction in food deserts to increase options.
Enhance data collection for resource allocation
The U.S. Department of Agriculture (USDA) measures food security through an annual survey. The survey asks respondents about their ability to afford food, how often they experience hunger and if they skip meals to save money. From this survey, the USDA determines the level of food security an individual or household may have, ranging from high food security to very low food security. To better understand areas of the state with very low food security, the CDC created a toolkit to asses transportation options, distance from grocery stores, income status and ratios of food retailers with healthy options. The toolkit outlines various data analysis needed to adequately determine areas of need. States and localities have created additional data programs to determine areas of need. For example, the Johns Hopkins Center for a Livable Future and the Baltimore Food Policy Initiative partnered to better understand food security in Baltimore. The program uses the Johns Hopkins’ Maryland Food System Map, which has 150 data indicators to determine areas with limited access to grocery stores while also looking at environmental conditions and clusters with social vulnerabilities. This work identified food deserts to address gaps in access and strengthen the local food economy. Governors can direct state agencies to tools like these and others like the United States Diabetes Surveillance System’s Social Vulnerability Index to better assess needs and allocate resources.
Expand food supplement programs
Governors can leverage programs to address challenged with food security in adults including Food is Medicine, Produce Prescription Programs and Meals on Wheels. To expand access for adults and families, Governors can address eligibility flexibilities for broad programs like SNAP, develop public-private partnerships and establish working groups to determine policy changes. Governors can also work with existing programs through grants and reimbursements to increase participation and delivery modes so more people experiencing food security challenges can be reached. In Michigan, Governor Whitmer signed Executive Order 2020-167, creating a food council to analyze the scope and causes of food security challenges and make recommendations to coordinate resources, take relevant legislative actions and assess evidence-based policies to decrease food security challenges.
Supplemental Nutrition Assistance Program (SNAP)
Formerly known as the Food Stamp Program, SNAP is a federal-state program designed to improve access to nutritious foods for people and households with low incomes. The federal government pays the full cost of SNAP benefits while the administrative costs are split between the state and federal government. Eligibility is determined by income level and value of assets, like a car. SNAP eligibility is set at the federal level; however, states have some flexibility to tailor eligibility. For example, New Jersey law allows SNAP registration by phone and allows seniors to register for Medicaid and SNAP simultaneously. Additionally, a Nebraska bill increased eligibility and allowed beneficiaries to adjust income and asset levels without losing benefits.
Partnering with state and local farmers and incentivizing growth of the state’s food industry
The federal government and various states have passed legislation to offer tax deductions and incentives to increase access to nutritious foods in communities experiencing high rates of food security challenges. The federal government offers enhanced tax deduction to all businesses (corporations, partnerships, sole proprietorships, etc.) if they donate food that meets specific criteria, such as donating the food to local food banks or other charitable organizations assisting people experiencing food security challenges. States can offer similar tax incentives and credits. For example, in 2013, former Iowa Governor Terry Branstad signed legislation establishing a tax credit for farmers who donate self-produced food commodities to food banks and food pantries. Governors can also incentivize growth of state-based food systems to increase access to a variety of fresh foods. In 2022, Alaska Governor Mike Dunleavy established a Food Insecurity and Independence Task Force through administrative order. The Task Force aims to advance the state’s food system by assessing barriers faced by the agriculture industry, providing recommendations to increase procurement of Alaska-sourced foods, developing a program to aid households impacted by fishery shortfalls and more. The Task Force collects data to determine administrative and statutory changes needed to achieve food security. These data will culminate in a report for the Governor, which is expected in September 2022.
Consideration Four: Increase Neighborhood and Physical Environment Walkability
The built environment is defined as the man-made structures where a population lives, works and plays. An analysis of the built environment often looks at walkability, or the degree to which an area is conducive to safely walking to amenities within a reasonable distance. Community designs that are walkable can allow residents to access safe and convenient sidewalks or paths that can get them to everyday destinations including grocery stores, schools, worksites and restaurants. According to a 2018 study, walkability is associated with lower risk for developing diabetes. In addition to walkability, populations with access to green spaces, like parks, gardens or playgrounds are more likely to be active and less likely to have diabetes or obesity. The Health and Human Services Community Preventive Services Task Force recommends park, trail and greenway infrastructure interventions combined with other interventions to increase physical activity. When communities added more parks and trails, use of parks or trails increased by 18.3%, and moderate to vigorous exercise increased by 17%. While there are positive health impacts of creating more green space, access issues still disproportionately affect certain populations. Racial and ethnic minority communities are three times more likely than White communities to live in nature-deprived places. Seventy-four percent of racial and ethnic minority communities live in nature-deprived places, and 23% of White communities live in nature-deprived places. Increasing greenspaces across the country can create healthy behaviors and reduce healthcare costs.
Governors can be leaders in promoting more walkable and green built environments by supporting, promoting and developing community plans that support active transportation. For example, Massachusetts Governor Charlie Baker and the Massachusetts Department of Transportation (MassDOT) launched the Complete Streets Funding Program in 2016 to encourage municipalities to design road networks that support physical activities such as walking and biking. The program consists of three tiers of participation. In the first tier, at least one representative from the municipality must complete a Complete Streets training and develop a Complete Streets policy that passes MassDOT scoring criteria. Tier two consists of the development of a Complete Streets Prioritization plan, which serves as a strategic roadmap for future projects. Lastly, the third tier is the construction of Complete Streets projects. To receive funding for construction projects, municipalities must first complete the first two tiers. Since the Complete Streets began, 280 municipalities have registered with the program. In 2022, Massachusetts was named the best state for bicyclists, largely due to the infrastructure built by Complete Streets.
Support and develop programs to look at the health impact of the built environment on diabetes outcomes
A Health Impact Assessment (HIA) helps to evaluate the public health impact of policies that may fall outside of traditional public health areas, such as transportation or land use. HIAs are tools that help communities and policy makers design communities that improve public health. HIAs can provide recommendations for policy makers on how best to increase positive health effects and minimize negative health effects. The major steps in a Health Impact Assessment are:
- 1. Screening: Identifying plan, project or policy decisions for which an HIA would be useful.
- 2. Scoping: Planning the HIA and identifying what health risks and benefits to consider.
- 3. Assessment: Identifying affected populations and quantifying health impacts of the decision.
- 4. Recommendations: Suggesting practical actions to promote positive health effects and minimize negative health effects.
- 5. Reporting: Presenting results to decision makers, affected communities and other interested partners.
- 6. Monitoring and evaluation: Determining the HIA’s impact on the decision and health status.
Governors can support HIAs by funding chronic disease and environmental health departments to work together on a HIA or supporting legislation that requires HIAs. For example, the Vermont Department of Health performed a health impact assessment to see the benefits of a State Employee Commuter Benefit Program. Vermont found that when transit commutes rose there was the potential for an increased rate of transportation-related physical activity and therefore a decreased risk of type 2 diabetes.
Strengthen promotion of physical activity through joint-use agreements in communities and jurisdictions
A joint-use agreement is an agreement executed between two government entities, typically a school and a city, to set the terms and conditions of shared use of public property or facilities. Often, these agreements are to share indoor and outdoor spaces like gymnasiums, athletic fields and playgrounds. This allows communities to share resources and have access to safe and free recreational spaces. The Governor’s office can support local jurisdictions going into joint-use agreements by creating materials and guides. For example, Tennessee’s state department of health created a Shared Use Agreement Handbook. This guide helps local health departments and communities create mutually beneficial joint-use agreements to create safe and affordable recreational spaces across Tennessee. The handbook has local community examples and copies of Tennessee laws and policies to assist communities that are working to establish recreational spaces.
Partner with physicians and outdoor recreation networks to prescribe outdoor exercise
According to a 2018 study, exposure to greenspace can lower the risk of many types of disease including type 2 diabetes. Governors can capitalize on these benefits by forming partnerships between healthcare systems, community organizations and park agencies to prescribe outdoor exercise to people at risk for diabetes. Capitalizing on this research, the National Parks Service, in partnership with the Golden Gate National Parks Conservancy, created National Park Rx as a way for health providers to encourage patients to spend time in nature. National Park Rx encourages providers to prescribe time in nature similarly to how they would prescribe medication. Prescribing time in nature can lead to positive health outcomes including weight loss, improving chronic conditions and lowering stress rates. Some states and localities have begun their own version of prescribing time in nature. For example, New Mexico has a program called Prescription Trails, a program that provides prescriptions for walking and wheelchair rolling routes in the community. The program came together through a partnership between the New Mexico Department of Health, Albuquerque Alliance for Active Living, New Mexico Health Care Takes on Diabetes and the National Parks Department. Prescription Trails has created an opportunity for physicians to partner with public health and built environment leaders to improve physical activity throughout the state’s population. Governors can encourage future partnerships like this in their states by connecting health departments with state outdoor recreation networks. The National Governors Association’s Outdoor Recreation Learning Network helps Governors and their outdoor recreation staff explore strategies to leverage access and promotion of states’ natural resources.
Learning Lab 3: Telehealth and the Healthcare System
Medical costs for people with prediabetes or diabetes are 2.3 times higher than people without diabetes. During the third learning lab, states discussed how they can be a part of the solution to reach people with diabetes throughout the country and provide them with comprehensive care.
Consideration Five: Support Innovative Health Care Practices to Create More Sustainable and Overarching Means of Care
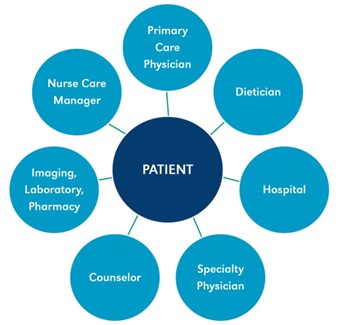
Health care providers are essential to averting the progression of prediabetes and the complications associated with type 2 diabetes. Governors can support culturally appropriate, innovative health care policies by engaging non-clinical providers and practices to support the patient-centered medical home model. The patient-centered medical home (PCMH) focuses on making primary care patient-centered, comprehensive, team-based, coordinated, accessible and focused on quality and safety. When used, a team-based PCMH can improve blood glucose, blood pressure and lipid levels in people with type 2 diabetes and can improve the value of care. By supporting policies that promote team-based care, states can create high-quality and efficient patient-centered care. Some barriers to integrating the PCMH model include gaps in health information systems and lack of accreditation processing.
Create systems that integrate non-physician healthcare workers into patient care
Governors can encourage systematic change to advance and ensure healthcare access from, including by focusing on Community Health Workers (CHWs) and pharmacists. CHWs understand the specific cultural aspects of the community through lived experience, training and consistent community engagement. They are often trusted within the community and work alongside other providers (medical providers, social workers, case managers, etc.) to integrate and coordinate client care. CHWs can offer coaching, social support and education to people with diabetes. Engaging CHWs can improve patients’ glycemic and lipid control and reduce their health care use by improving the patient’s ability to navigate their diagnosis. State officials can encourage the engagement of CHWs to better understand their immense expertise and determine where they fit in the larger health care system. Governors and state health officials can engage CHWs by investing in the CHW workforce. Some states have explored using Medicaid to finance CHW-delivered services. For example, Illinois HB 158 established that certain services delivered by CHWs working under the supervision of a Medicaid-enrolled provider will be covered under its Medicaid program. Governors can work with their state legislature and Medicaid programs to extend reimbursement and benefits for CHWs.
Pharmacists can also be a piece of the team-based care puzzle as they are one of the more accessible health care professionals. With 91% of all prescriptions filled by people with chronic disease, pharmacists are well positioned to engage people who have or are at risk for developing diabetes. One way the Governor’s office and state health department can utilize pharmacy care is to convene pharmacy schools and professional organizations and create programming to integrate pharmacists in diabetes prevention and management. For example, as part of a cooperative agreement funded by CDC, Alabama’s Department of Public Health partnered with the Samford School of Pharmacy to provide training for pharmacies on diabetes self-management education and support services (DSMES) accreditation. By partnering with pharmacies, states can expand knowledge networks and spread information on type 2 diabetes prevention and management tactics.
Utilize surveillance systems to assist physicians in reaching hard-to-reach populations
Electronic health information exchanges (HIE) allow physicians and other health care providers to exchange vital medical information electronically. By sharing information electronically, health care teams can better track diabetes risk factors such as high BMI or A1C levels and assist patients in improving their health. HIEs can also be used as a statewide program to track population health. MarylandCRISP (Chesapeake Regional Information System for Our Patients), the state designated HIE for Maryland, facilitates the electronic transfer of clinical information between disparate health information systems. During the State Strategies to Prevent and Manage type 2 Diabetes Learning Lab, the Maryland Medicaid Administration shared information about their collaboration with CRISP through funding from the CDC to create a prediabetes flag for clinicians. If a Medicaid patient likely meets the criteria to be at risk for diabetes, the CRISP system will automatically send a Care Alert to the physician who can take appropriate action to address the condition and refer the patient to the National DPP. The flag also enables population-based reporting on individuals who are at risk for Type 2 Diabetes in support of the Maryland Total Cost of Care Model’s population health goal related to diabetes prevention, as well as in support of the Maryland Department of Health’s Diabetes Action Plan. Through the prediabetes flag, physicians can closely track a patient’s risk for developing diabetes and work with these populations closely to reverse the risk factors.
Engage with umbrella hub organizations to assist community-based organizations with National DPP reimbursements
One barrier that small, community based National DPP providers may encounter is a lack of capacity to perform administrative duties to receive insurance reimbursement from CMS or other payers. CDC has created umbrella hub arrangements to reduce the administrative burden by connecting community-based organizations (CBOs) to each other. Umbrella hub arrangements can aid organizations in achieving sustainability so they can continue to deliver the National DPP to populations who need it most. Governors and state health officials can promote these arrangements by encouraging meetings and webinars to increase awareness among Medicaid officials, health care providers, and other interested partners.
Consideration Six: Use telehealth to engage hard–to–reach populations
Telehealth can supplement in-person services and address health access disparities. People who are at higher risk of developing type 2 diabetes often experience barriers to receiving in-person care. For example, rural populations are at an increased likelihood of developing type 2 diabetes and experience access issues, such as having fewer health care and transportation providers available to them. Utilizing telehealth in diabetes prevention and management can increase the accessibility of not only appointments with providers, but also access to programs like the CDC’s National DPP lifestyle change program or Diabetes Self-Management Education DSMES services. Access to health care and education via telehealth can minimize gaps in care and give resources to a larger subset of the population. Telehealth does not sacrifice outcomes, as studies have shown that providing the National DPP and DSMES services via telehealth is as effective as in person services. However, there are barriers to expanding telehealth. Telehealth is not always covered by insurance. If telehealth is covered, providers are not always reimbursed at the same rate as in person services, disincentivizing providers from offering telehealth services. In addition, provider licensing requirements prevent providers from practicing across state lines. Many populations lack access to broadband which may also hinder their ability to utilize telehealth care. NGA has previously published a paper titled The Future of State Telehealth Policy, which gives a more comprehensive overview of state policy levers to increase telehealth and can be adapted to address diabetes specifically.
Support telehealth service coverage both for Medicaid and commercial insurance
To reduce the impact of type 2 diabetes on populations with low incomes, Governors can support Medicaid coverage for virtual delivery of the National DPP lifestyle change programs and DSMES services. States have the flexibility to determine many key areas, including which Medicaid populations can receive services via telehealth, which services can be delivered remotely and how services will be reimbursed. States also decide which types of providers can deliver services via telehealth, which modalities can be used, and the rules governing managed care plans. When making these determinations, Governors may consider including coverage for type 2 diabetes prevention and management across a broad scope of populations and provider types, including coverage for online or distance learning of the National DPP lifestyle change program and DSMES. To obtain Medicaid coverage, a state plan amendment is only required if services provided by telehealth are paid at different rates than in-person services; otherwise, a statute is sufficient.For example, Montana’s Medicaid Program used a state plan amendment to establish coverage and reimbursement for the National DPP in 2009. Since enacting the state plan amendment, Montana has established 13 telehealth sites that offer the National DPP. Additionally, Governors can work with their state legislatures to require private payer insurance plans to reimburse for services provided via telehealth. Policy levers include state laws that either require coverage parity, payment parity, prohibit insurers from requiring a previously established provider-patient relationship, protect enrollees from unfair cost-sharing and more.
Build on licensing and reimbursement flexibility in place during the COVID-19 state of emergency
The COVID-19 pandemic increased access to telehealth services. States implemented regulatory waivers for Medicaid or all payers that allow telehealth providers to practice across state lines and require parity between coverage and payment. Governors can engage interested partners to determine continuation of those flexibilities. Before the COVID-19 pandemic, states required out-of-state providers to be licensed in the state where they were providing services. Arizona, West Virginia, Kansas and Connecticut made their regulatory waivers permanent. Licensing compacts are another option for states. The Interstate Medical Licensure Compact (IMLC) allows participating states to administer telehealth services across state lines by creating an expedited path to licensure. To date, IMLC includes 33 states, the District of Columbia and Guam. Since the COVID-19 pandemic began, Texas, Delaware and Ohio have joined the compact and compact legislation has been introduced in Missouri, Virginia, North Carolina, Massachusetts, Connecticut and Rhode Island. Payment parity between telehealth and in-person care also emerged as a key issue during the COVID-19 pandemic. Payment parity encourages providers to use telehealth by guaranteeing the same payment or reimbursement rate. Before COVID-19, only ten states required parity for all payers and four states required parity for Medicaid. During the public health emergency, 19 states required parity for all payers and 14 states required parity for Medicaid. Eighteen states have since made telehealth parity permanent for all payers and six states for Medicaid. Several federal telehealth flexibilities are also becoming permanent. Other flexibilities surrounding coverage for telehealth through Medicaid are up to the states, including coverage of telehealth services via telephone, electronic and virtual means, home as the originating site and asynchronous telehealth services. For example, in the 2022 learning lab, Alaska mentioned that their National DPP allowed telephonic attendance to improve broadband access.
Create initiatives to address broadband access as a social determinant of health
The COVID-19 pandemic illuminated the importance of broadband access as a social determinant of health. Type 2 diabetes prevention and management via telehealth can only be successful if individuals have access to the internet. Individuals without access to broadband are disproportionately low-income, older, living in rural areas and members of racial and ethnic minority communities. In 2020, at least 18.3 million people in the U.S. lacked access to sufficient broadband, and 14 million of them lived in rural areas. This can further exacerbate health disparities and inequities, as many people who do not have access to broadband also face other barriers to care including a lack of transportation or insurance. To ensure telehealth is equitable, it is important to implement policies that increase access to high-quality, affordable broadband. In addition to federal funding opportunities to expand broadband access, including recent investments from the Infrastructure Investment and Jobs Act (IIJA), Governors have created other funding allocations and broadband initiatives. For example, Iowa invested $85 million from The Coronavirus Aid, Relief, and Economic Security Act to expand telework, telehealth and remote learning through broadband expansion. The state also allocated $50 million in grants for broadband infrastructure expansion through the Rural Iowa Broadband Grant Program and the Iowa Communication Network, which resulted in upgraded equipment at 71 hospitals and clinics to accommodate increased telehealth services. NGA has developed a number of resources on broadband, including Broadband Affordability Resources, Governor Strategies to Expand Affordable Broadband Access and others available through our website.
Learning Lab 4: Diabetes Management and Medication
In learning lab 4, states and subject matter experts discussed how to reduce morbidity and mortality that occurs from Type 2 diabetes. States thought through how to increase access to programs that help people with diabetes manage their diagnosis and how to decrease the burden of drug pricing for those who need medication.
Consideration Seven: Increasing referrals to Diabetes Self-Management and Education Services
DSMES or diabetes self-management education and support services are designed to give people with diabetes the knowledge and skills to responsibly manage a diabetes diagnosis. DSMES helps individuals maintain healthy lifestyle habits including healthy coping, healthy eating and being active, which can result in fewer or less severe complications and decreased health care costs. Studies have shown that completing more than 10 hours of DSMES over the course of 6-12 months led to a significant reduction in average blood sugar levels (A1C), compared to those who spent less time with diabetes and education specialists. Despite proven health improvements in those who utilize DSMES services, DSMES is significantly underutilized with only 6.8% of privately insured individuals with diabetes using these services within 12 months of diagnosis. Barriers to increasing knowledge and utilization of DSMES services include a lack of insurance coverage for the program and lack of provider knowledge.
How Do You Manage Type 2 Diabetes?
The ADCES Self-Care Behaviors serves as a person-centered approach for people with diabetes to self-manage their diagnosis
- Healthy Coping
- Healthy Eating
- Being Active
- Taking Medication
- Monitoring
- Problem Solving
- Reducing Risks
Expand access to DSMES through Medicaid Coverage
States have used a variety of mechanisms to provide Medicaid coverage for DSMES. As of 2019,15 states have laws that require their state to cover DSMES, 18 states cover DSMES through sub-regulatory Medicaid materials including administrative codes, Medicaid state plans and waivers, and one state provides DSMES through MCOs. During the NGA learning lab, subject matter experts developed steps states without DSMES coverage can take to create a pathway to coverage DSMES coverage.
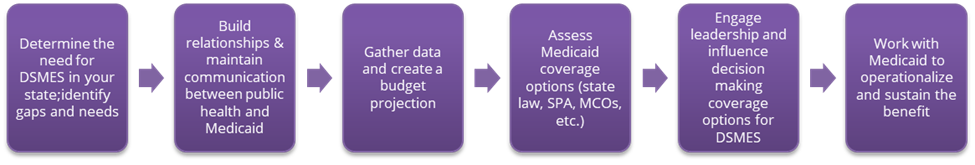
Through their executive power, Governors can support public health and Medicaid officials in covering DSMES. For example, Governors can provide funding to look at the burden of diabetes in their state and determine the need for DSMES. In Delaware, the Diabetes Burden Report for 2021 advocated for expanded coverage policy of DSMES with private and public insurers, with an emphasis on Medicaid recipients, as well as state and public employees. Further, The Impact of Diabetes in Delaware 2019 includes recommendations to continue to fund statewide awareness campaigns and targeted outreach for DSMES to high-risk populations in the state including Delaware Medicaid and Group Health Insurance (GHIP) beneficiaries.
Identify and address barriers to provider referrals
Increasing provider knowledge and referrals to DSMES can increase the number of people with diabetes who receive services. Barriers noted by providers include confusion about DSMES services referrals and daunting referral forms and paperwork. States can address this confusion by developing electronic health record programs that can track referrals, identify people with diabetes in need of follow ups and close referral loops between providers and DSMES services. Another way electronic health records can aid linkage to care is through a provider referral network. A provider referral network is an electronic health record system that enhances and streamlines communications amongst providers as they refer patients to the DSMES. Referral networks can increase utilization of DSMES and allow providers to address personal barriers that participants might have early on. Having referral and provider relations champions in the Governor’s office or in state or local health departments can encourage the providers who interact with people with diabetes (including dieticians, retinopathy specialists, podiatrists, pharmacists and mental health providers) to encourage patients to participate.
Consideration Eight: Increase Transparency to Lower the Cost of Diabetes Care
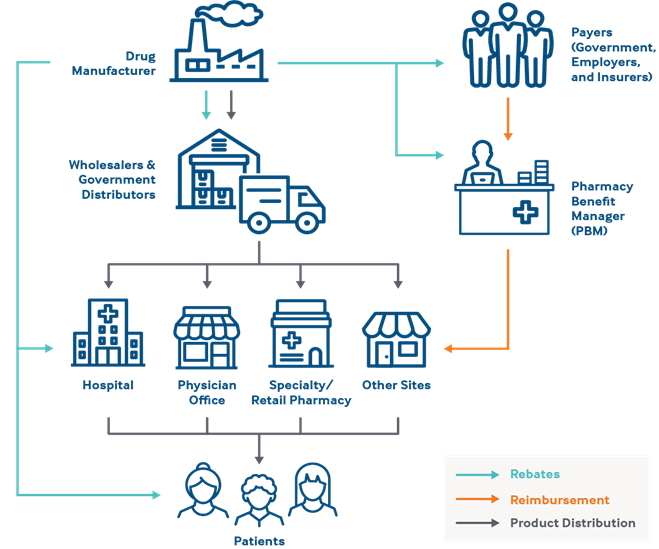
Unmanaged diabetes can lead to severe complications, including kidney damage, blindness and increased risk for heart disease and stroke. This has a high cost for both the individual and the community, with an estimated $90 billion lost due to reduced productivity caused by diabetes. Out of 37.3 million Americans with diabetes, approximately 7.3 million rely on insulin to manage their condition. Insulin prices increased exponentially, with one vial of insulin costing $21 in 1999 and $332 in 2019, reflecting a price increase of more than 1,000% after adjusting for inflation. With this increase, as many as 1 in 4 people with diabetes report rationing insulin to save money. Rationing medicine can lead to negative health outcomes; a 2019 study found patients who rationed insulin were three times more likely to have poor blood sugar control than those who did not have to ration. Governors can champion policies that improve transparency in the pharmaceutical supply chain, which establishes accountability for the players in the supply chain and can lead to less price increases. For example, in 2017 Nevada passed price transparency legislation requiring pharmaceutical companies and pharmacy benefit managers to report costs associated with production, sales and profits of essential drugs used to manage diabetes. Governors can also form task forces focused on developing ideas to lower the cost of prescription drugs.
Insulin copay caps
Several states have implemented insulin copay caps. Insulin copay cap laws set a maximum price on private insurance copays to decrease out-of-pocket costs for people with diabetes. As of June 2022, 20 states have implemented a monthly copay cap for insulin ranging from $25 to $100 per 30-day supply of insulin Additionally, the 2022 Inflation Reduction Act reduced Medicare Part D beneficiaries’ out-of-pocket spending on insulin at $35 per month. Governors who support copay caps can work with their legislature to champion this policy and others that decrease out of pocket costs for people with diabetes.
Drug rebate pass through
States can also work to regulate drug pricing at the pharmacy benefit manager level. Pharmacy benefit managers (PBM) are companies that manage prescription drugs and negotiate drug pricing with manufacturers and pharmacies. PBMs work on behalf of health insurers, Medicare Part D drug plans, large employers and other payers. Traditionally, PBMs engage in spread pricing, where they contract with health plans to manage their prescription drug benefits and keep a portion of the amount paid to them by the health plans for prescription drugs instead of passing the full payments on to pharmacy. If spread pricing is not monitored, a PBM can charge an excess amount to health plans, which can lead to higher prescription prices overall. States can implement “pass through pricing,” under which PBMs receive a flat fee for each prescription it processes and are paid a set amount per prescription. The pass-through model can help make the pharmaceutical supply chain process more equitable. In 2021, West Virginia was the first state to implement a pass-through model. The legislation requires insurance companies and PBMs to automatically account for the savings that they receive by calculating what a patient pays at the pharmacy.
Bulk purchasing
States can purchase pharmaceuticals in bulk or join a purchasing pool to lower the unit price of a drug and increase access to medication. Bulk purchasing has been used both by federal and state government entities to purchase vaccines and medications used to treat infectious diseases such as HIV or Hepatitis C. Three multistate Medicaid drug purchasing programs currently exist with a total of 30 states participating. These purchasing programs create savings by generating a preferred drug list (PDL), which is a catalog of outpatient drugs that states encourage providers to prescribe over others. This allows state departments of health to negotiate higher supplemental rebates. A state may attach a higher copay or require prior authorization for drugs not on the PDL. In 2022, Washington’s healthcare authority collaborated with the legislature to create a program where the state’s Medicaid program could establish partnerships with another state, group of states, state agency, a nonprofit, or any other entity to produce, distribute or purchase insulin and generic prescription drugs. Once purchased, local governments, private entities, health carriers and others in Washington may choose to voluntarily purchase the generic prescription of drugs and insulin from the authority as available quantities allow.
Conclusion
Type 2 diabetes affects millions of people across the United States, and the prevalence of diabetes is increasing each year. Social determinants of health are primary factors affecting one’s ability to manage diabetes and reduce risk of severe complications. People with diabetes who may have low-incomes, be older or live in underserved communities can be assisted through comprehensive local and state programs, such as those discussed throughout this paper. Key partnerships facilitated by the Governor can lead to innovative services that address direct issues, like out-of-pocket insulin costs, and underlying factors like socioeconomic status, health inequities and disparities, food security challenges, lack of safe housing and racism. Governors can help their constituents, while also saving the state money in the long run, by exploring and implementing some of the strategies outlined in the publication.
Acknowledgements
The National Governors Association Center for Best Practices (NGA Center) would like to thank the state officials and other experts who offered insights that informed this publication. A special thank you goes to the participants in the NGA Center Learning Lab on State Strategies to Prevent and Manage Type 2 Diabetes and to the team at Leavitt Partners who partnered with the NGA Center on delivering the learning lab sessions.
The NGA Center would also like to thank the Centers for Disease Control and Prevention (CDC) for their generous support of the learning lab and this publication under this cooperative agreement. This web resource is part of a project funded by the CDC Division of Diabetes Translation. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the CDC or the U.S. Department of Health and Human Services.
This publication was developed by NGA Center for Best Practices Policy Analyst Myra Masood. This publication has contributions from CDC Public Health Associates Eden Moore and Taylor Shelton; Senior Policy Analyst, Michelle Leblanc; and Program Director Brittney Roy.