In a time when the drug supply is more lethal than ever, preventing substance use and mitigating risk among youth is a critical bipartisan priority.
(Download)
Mental health conditions and substance use are inextricably linked, and during a time of concurrent overdose and youth mental health crises, Governors are working to protect and support youth with multi-disciplinary and strategic approaches that invest in root cause prevention and improve access to high-quality services. The presence of mental health conditions, trauma or neurodevelopmental disorders increases a person’s risk for developing a substance use disorder. Alarmingly, overdose deaths among adolescents increased 109% from 2019 to 2021. States are taking actions to acknowledge the connection between these crises and enhance upstream protective factors and youth mental health services, which will have rippling impacts in preventing substance use. Many Governors are also enacting policy solutions and investing in programs to mitigate harms amidst a dangerous drug supply as part of a comprehensive strategy, keeping youth alive until they can access the services and support they need. These approaches are critical in this third wave of the United States overdose epidemic where fentanyl dominates the drug supply, and substance use can result in fatal overdose even in the absence of frequent use or addiction.
Mental Health Conditions as Predictors of Substance Use and Overdose Risk in Youth
Mental health disorders, experiences of trauma and neurodevelopment disorders in youth are strong predictors of substance use, earlier first use and development of substance use disorder (SUD) later in life. Among young people who fatally overdosed between July 2019 and December 2021, 41% had a mental health condition or treatment history. People with Attention Deficit Hyperactivity Disorder (ADHD), Autism Spectrum Disorder (ASD), depression, bipolar disorder, obsessive-compulsive disorder, as well as certain personality traits have increased odds of developing SUD. In addition, the impact of Adverse Childhood Experiences (ACEs) on mental health and substance use is well-known. Medicaid-enrolled youth and youth of color who have mental health and developmental disorders face additional challenges and risk factors. Adolescents living in poverty have a higher prevalence of mental health conditions than youth from families with higher socioeconomic backgrounds.
Examining the reasons youth use substances can provide insights into the link between mental health disorders and substance use. Youth may use substances for many reasons including social motives, sensation-seeking, as well as trauma-related self-medication. Consider ADHD, the most prevalent neurodevelopmental disorder among children, which strongly predicts substance use and is more prevalent among children with ACEs and those living in poverty. It is even more strongly linked to substance use when comorbidities exist with autism spectrum disorder or mood disorder (e.g., bipolar, depression). Between impulsivity, risk-taking behavior, social isolation, difficulty fitting in and challenges with academic achievement, youth with ADHD and other mental health conditions may find themselves experimenting with substances to fit in, to cope and to self-medicate.
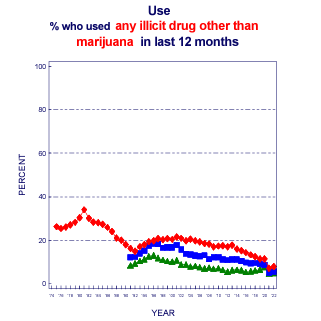
It has never been more dangerous to use illicit drugs given the current landscape of the drug supply. Youth with mental health conditions that affect their impulsivity are likely to take risks with using and continuing to use substances despite the context of a dangerous drug supply, even when others might not. In 2021, 7.2% of 12-grade youth reported using an illicit drug other than marijuana in the past year, the lowest rate since the data has been collected, and youth use of illicit drugs overall has remained stable or dropped in recent years. Fentanyl drives most fatal overdoses and is used in counterfeit pills, which mimic the appearance of prescription grade medication—including opioids, stimulants and other classes of drugs. Even with historically low rates of substance use among adolescents, youth can fatally overdose without a diagnosable substance use disorder or frequent use. Any use is a potential risk; among overdose decedents between July 2019 and December 2022 aged 10-19, two out of three had no history of opioid use.
Mitigating the Link Between Mental Health Conditions and Substance Use in Youth
Preventing Adverse Childhood Experiences and Strengthening Protective Factors
Because mental health and substance use are strongly linked, focusing on the root causes of mental health disorders will reduce substance use and overdose. Governors are committed to improving youth mental health and preventing and mitigating substance use. NGA Chair New Jersey Governor Phil Murphy’s NGA Chair’s Initiative focuses on strengthening youth mental health, and substance use was a frequent priority identified in numerous Governors’ 2023 State of the State addresses. Governor initiatives to strengthen families also support these goals, as parent and family engagement and family support are protective factors that prevent youth substance use.
Governors are leading the way on preventing Adverse Childhood Experiences (ACEs) and mitigating the effects of trauma in coordination with mental health and substance use disorder (SUD) services. In 2020 and 2021, four states participated in an NGA Learning Collaborative, culminating in the release of a report in 2021 looking at preventing and mitigating ACEs. The Learning Collaborative also led to the formation of the State Trauma and Resilience Network, a group of 11 states working together to promote best practices around trauma-informed care and ACEs mitigation, including linkages to SUD prevention.
Ensuring Access to High-Quality Services
Early detection and linkage to care for mental health conditions, as well as substance use, can ensure youth access the support and treatment they need. Accessing early treatment for mental health conditions leads to better health outcomes and overall better quality of life. Detecting and treating mental health conditions early has the potential to mitigate the relationship between mental health conditions and substance use disorders.
The large share of adolescents and youth covered by Medicaid and CHIP presents an opportunity for early detection in a high-risk population. States can leverage federal guidance and resources to provide high-quality behavioral health services, including screening, to this population. The Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit of Medicaid and CHIP can help states increase detection of mental health disorders and connect youth with treatment. Consistent implementation and compliance with EPSDT guidelines vary between states. Centers for Medicare & Medicaid Services (CMS) issued an informational bulletin in 2022 to remind State Medicaid Agencies about EPSDT requirements, emphasizing its role in addressing the youth behavioral health crisis and citing several resources, opportunities and examples. The Colorado General Assembly is considering a bill to provide access to behavioral health services for youth Medicaid recipients without requiring a diagnosis, demonstrating a commitment to preventive behavioral healthcare.
State efforts to address behavioral health workforce shortages will also ensure more youth with mental health and substance use disorders get help. The dearth of behavioral health providers for youth, particularly those who accept Medicaid/CHIP, contributes to access challenges. In the meantime, states can implement and support policies that enhance access to telehealth, which can connect youth with behavioral health services in the absence of nearby high-quality services.
Reducing Substance Use-Related Harms and Preventing Overdose

It is critical for states to supplement ACEs and substance use prevention efforts with strategies that reduce risks, given the potential for overdose even in the absence of diagnosed substance use disorder and context of low substance use rates among youth. Many Governors have launched awareness campaigns around the Drug Enforcement Administration mantra “One Pill Can Kill” to raise awareness of the dangers, particularly among youth and teens. These campaigns help inform youth’s perception of the dire risks associated with illicit drug use. However, youth with mental health conditions may be predisposed to take risks even when they are aware of these dangers.
Governors can continue to invest in targeted overdose education and naloxone distribution initiatives to prevent fatal overdose among youth. Overdose education and naloxone distribution can target parents, particularly those with children who have mental health conditions that put them at increased risk for substance use. Over 60% of youth overdoses happen at home; in most cases, there is no documented overdose response from a bystander (67.8%). Many schools already keep naloxone onsite to respond to overdose emergencies, a strategy the National Association of School Nurses endorses.
Overdose education and naloxone distribution can also be implemented through policy change and cross-agency collaboration with systems that serve youth likely to have mental health conditions and trauma histories. For example, the Arizona Department of Child Safety has a policy requiring naloxone onsite for foster homes, group homes and other facilities serving youth. A partnership in New Mexico between the Children, Youth & Families Department and Human Services Department provides training on overdose response and issues naloxone to juvenile probation officers, transition coordinators, community behavioral health therapists and staff who work in juvenile justice facilities.
Fentanyl test strip distribution is another evidence-based strategy that could help youth reduce overdose risk when using illicit drugs. Kansas Governor Laura Kelly recently discussed decriminalizing test strips in the state at a roundtable with a parent who had lost a child to fentanyl overdose. Mississippi, Ohio and South Dakota are some of the most recent states to pass legislation allowing for the distribution of fentanyl test strips.
In a time when the drug supply is more lethal than ever, preventing substance use and mitigating risk among youth is a critical bipartisan priority. Adequately addressing youth behavioral health requires a multi-disciplinary and strategic approach, and Governors are uniquely positioned to fund and implement policy solutions that improve mental wellness, prevent trauma and reduce youth substance use and overdose. By ensuring quality and accessibility of services and tools that promote mental wellness and reduce risks, states can reduce adverse outcomes associated with substance use in youth.
This issue brief was written by NGA staff Dana Heilman and Marianne Gibson. To learn more about these topics, please contact Dana Heilman (DHeilman@nga.org).