State Health Workforce Toolkit
Profession-Specific Resources
Introduction
Direct care workers, such as nursing assistants, home health aides, personal care aides, and direct support professionals, are a critical component of the health workforce that serves older adults and people affected by disabilities. COVID-19 has heightened awareness of existing challenges to the recruitment and retention of direct care workers. The demand caused by COVID-19 and other population health challenges as well as the new funding opportunities provided as a result of COVID-19 have created urgency for solution development. Several states and employers have made great strides in developing strategies to support their direct care workforce.
Presented below is information provided for governors and their administrations to review and consider as states begin to understand the current state of their direct care workforce and begin to develop actionable state solutions.
Actions for Governors:
- Determine who in your state might need to be engaged in direct care workforce conversations and strategy development by generating an Inventory of Direct Care Workforce Stakeholders
- Understand the current landscape of the direct care workforce in your state by reviewing Common Direct Care Roles, associated laws or regulations, and any workforce data that may be accessible to quantify these workers.
- Explore Direct Care Workforce Development strategies such as registered apprenticeships, work-based learning opportunities, and career pathways, and consider whether these strategies may be appropriate for your state.
- Conduct a Direct Care Workforce Wage Assessment to understand the current state of wages for this workforce in your state compared to living wage estimates.
Inventory of Direct Care Workforce Stakeholders
Purpose
The first consideration in the Issue Brief State Strategies for Sector Growth and Retention of the Direct Care Workforce is “Work across state agencies and with employers and academic institutions, such as community colleges, to identify priorities and coordinate in the development of pipeline and workforce development programs.”
As states take an organized approach to direct care workforce (DCW) planning, a helpful early step is generating a list of the various stakeholder perspectives. The following template can be used to identify and organize stakeholders by the role they serve in direct care workforce conversations. Such an inventory could support coordination of related initiatives, whether informal or formalized.
Common Direct Care Workforce Stakeholder Perspectives by Role
*Note: The list of stakeholder perspectives below was developed after reviewing membership from state direct care workforce workgroups. These perspectives are presented for consideration and should not be considered exhaustive.
State Government - Executive Branch
| Perspective | Common Role in DCW Conversations |
|---|---|
| Licensure boards or other entities that regulate or have jurisdiction over direct care workers |
|
| Workforce development or labor agencies and any relevant boards or committees |
|
| Departments of education, higher education, career and technical education |
|
| Public health and human services agency (which may include specific contacts related to following agency activities: facility licensing, provider licensing, health care quality) |
|
| Medicaid Agencies (which may include specific contacts related to the following agency activities: provider reimbursement, aging, disabilities, mental health, etc.) |
|
| State-based councils or forums | Some states have councils or forums related to the DCW overall or focused on special populations (such as disabilities or aging) |
State Government - Legislative Branch
| Perspective | Common Role in DCW Conversations |
|---|---|
| Health | Legislation and oversight related to a number of areas of health care, generally including direct care occupational regulation and Medicaid. |
| Labor | Legislation and oversight related to labor, employment, workforce, economic development, etc. |
| Appropriations/Budget/Ways and Means | Considers legislation involving expenditure of state and federal funds, including developing the state’s budget with appropriations for state agencies, departments, and organizations. This likely includes any strategies related to direct care wage. |
External - Employers/Payers of DCW Services
| Perspective | Common Role in DCW Conversations |
|---|---|
| American Health Care Association/National Center for Assisted Living State Chapter | Association representing long term and post-acute care providers, including: non-profit and proprietary skilled nursing centers, assisted living communities, sub-acute centers and homes for individuals with intellectual and developmental disabilities |
| Leading Age | Association representing aging service providers |
| The ARC | Community-based advocacy organization for individuals with intellectual and developmental disabilities (these individuals may serve as consumer-employers of DCW or may receive DCW services) |
| Long-term Care Insurance | Payer of DCW services |
| Major Insurers/Managed Care | Payer of DCW services, may be responsible for DCW network adequacy measures |
| National MLTSS Health Plan Association | National organization that supports Medicaid managed long-term services and supports (MLTSS) and integrated care for dually eligible beneficiaries. |
| American Hospital Association | “National organization that represents and serves all types of hospitals, health care networks, and their patients and communities.” |
External - Consumers of DCW Services
| Perspective | Common Role in DCW Conversations |
|---|---|
| Area Agencies on Aging/USAging | Supporting local Area Agencies on Aging and representing older adults and people with disabilities |
| Alzheimer’s Association | Represents individuals with Alzheimer’s that may receive DCW services |
| The ARC | Community-based advocacy organization for individuals with intellectual and developmental disabilities (these individuals may serve as consumer-employers of DCW or may receive DCW services) |
| AARP | Represents aging individuals |
| Individual Consumers | Consumers of DCW services |
External - Pipeline/Educators/Trainers of DCW
| Perspective | Common Role in DCW Conversations |
|---|---|
| Community Colleges | Community Colleges commonly provide education/training and/or testing services for entry into DCW roles |
| Area Health Education Center | AHECs may serve as pipeline support for DCWs by working with K12 students or pre-professional health care students |
| HOSA | State HOSA chapters may have connections with secondary, postsecondary, middle school, and adult learners interested in health care careers |
| Career and technical training entities | Many states have developed state-approval processes for DCW training. Approved training entities may be key stakeholders. |
| Higher Education Institutions | Career ladders may be developed from DCW roles to those touching the higher education sector. |
External - DCW/Provider Associations/Representatives
| Perspective | Common Role in DCW Conversations |
|---|---|
| Direct care workers or caregivers | Provide DCW services |
| Service Employees International Union (SEIU) or other unions | Represent the workforce providing services to individuals with intellectual or developmental disabilities |
| National Alliance for Direct Support Professionals (NASDP) | Represent the workforce providing services to individuals with intellectual or developmental disabilities |
| National Association for Home Care & Hospice | Organization representing home care and hospice organizations and their workforce. |
| Paraprofessional Healthcare Institute (PHI) | Direct care workforce research and advocacy |
| ADvancing States | “ADvancing States supports visionary leadership, the advancement of systems innovation and the articulation of national policies that support long-term services and supports for older adults and people with disabilities.” |
Common Direct Care Workforce Roles and Associated Workforce Data
Purpose
The second consideration in the Issue Brief State Strategies for Sector Growth and Retention of the Direct Care Workforce was “Compare, standardize and streamline roles and regulatory requirements for direct care worker roles across state agencies.”
As states seek opportunities to streamline direct care workforce roles and policies, an important first step is understanding who the direct care workforce is, how many direct care workers there are in a state, and what policies are in place that impact direct care worker entry and practice requirements. Below is a template that states could use to identify, quantify, and define their direct care workforce.
Common Direct Care Roles
Nursing Assistants

- Who they are: Nursing assistants commonly work in facility-based settings such as nursing homes, addiction recovery centers, and physical rehabilitation centers.
- Associated federal and state regulations: Federal legislation and associated regulations outline minimum training requirements for nursing assistants that provide services in Medicaid or Medicare-facilities, which is 75 hours of training, of which at least 16 hours must be clinical or in-service training. States may go above and beyond this federal minimum. Federal regulations also require that states establish and maintain a registry of nursing assistants.
- Workforce data and tracking: To determine how many nursing assistants are in a state, states could use the registry to quantify the number of nursing assistants practicing in CMS nursing facilities. State registries typically include personally identifiable information (name, date of birth, etc.) and in some instances may include additional demographic information (example: race and ethnicity). However, registries typically do not include current employment information for nursing assistants. Nursing assistants are required to routinely renew their state certification to remain on the registry. Some states collect additional information, such as employment status and employment plans, from nursing assistants as part of the renewal process to support workforce assessments and planning. Alternatively, states may find value in reviewing labor data from the Bureau of Labor Statistics (BLS) associated with Standard Occupational Classification (SOC) 31-1131.00 (Nursing Assistants). BLS data likely includes both those nursing assistants on the registry as well as those providing similar services in non-nursing home settings.
Many states have provisions for an advanced nursing assistant that can administer certain types of medications under delegation and supervision of a licensed nurse. These roles are commonly referred to as “medication aides” or “medication technicians” and generally require additional training, experience, and testing. A review of these roles and associated regulations was conducted by the American Nurses Association and can be found here.
Home Health Aides

- Who they are: Home health aides commonly provide healthcare support services in a home-based setting.
- Associated federal and state regulations: Federal legislation and associated regulations outline minimum training requirements for home health aides employed by Medicare-certified home health agencies, which is 75 hours of training, of which at least 16 hours must be supervised practical or in-service training. States may go above and beyond this federal minimum. Federal regulations also require that states establish and maintain a registry of home health aides.
- Workforce data and tracking: To determine how many home health aides are in a state, states could use the registry to quantify the number home health aides employed by Medicare-certified home health agencies. State registries typically include personally identifiable information (name, date of birth, etc.) and in some instances may include additional demographic information (example: race and ethnicity). However, registries typically do not include current employment information for home health aides. Home health aides are required to routinely renew their state certification to remain on the registry. Some states collect additional information, such as employment status and employment plans, from nursing assistants as part of the renewal process to support workforce assessments and planning. Alternatively, states may find value in reviewing labor data from the Bureau of Labor Statistics (BLS) associated with Standard Occupational Classification (SOC) 31-1121.00 (Home health aides). BLS data likely includes both those home health aides on the registry as well as those providing similar services under other employers.
Personal Care Aides

- Who they are: Personal care aides commonly provide personal services to support activities of daily living either in a facility-, community-, or home-based setting. Personal care aides may be referred to under many different titles, including personal care attendant, home care worker, direct service worker, and many more. Personal care aides may focus on a number of specialty populations such as those individuals with intellectual disabilities, physical disabilities, behavioral disorders, or aging populations.
- Associated federal and state regulations: There are not currently any federal regulations outlining minimum training requirements for personal care aides. However, a number of states have adopted state minimum training requirements. There are no federal requirements for development or maintenance of a registry.
- Workforce data and tracking: There are no federal requirements for states to maintain a registry of Personal Care Aides. Therefore, most states do not have a repository of information on all personal care aides. However, if states do implement minimum training requirements, there may be an opportunity for states to quantify the number of these workers through assessing personal care aide training completion and/or certification (if implemented). Alternatively, states may find value in reviewing labor data from the Bureau of Labor Statistics (BLS) associated with Standard Occupational Classification (SOC) 31-1122.00 (personal care aides).
Direct Care Workforce Development
Purpose
The third consideration in the Issue Brief State Strategies for Sector Growth and Retention of the Direct Care Workforce is “Identify and support training opportunities that enhance accessibility of direct care jobs and create opportunities for career growth.”
Direct care jobs typically require limited training and education and therefore can serve as an accessible entry point for work in the health sector. Although demand for these roles is high and their services are critical, many states may not prioritize these roles in workforce development initiatives because the wages typically fall below thresholds set by states for inclusion in such initiatives. To address this issue, state education and workforce initiatives can be focused on ensuring these roles are only the first step on a clear career pathway that leads to higher wage opportunities. There are several solutions states may implement to address training needs, support recruitment, and build pathways for career progression. These strategies include: apprenticeships, work-based learning opportunities, and career pathways.
As states explore the progression of direct care workforce development strategies, a first step may be to assess current direct care workforce development programming. Below is a toolkit that states may use to understand the current state of direct care workforce development initiatives and explore opportunities to enhance these strategies.
Registered Apprenticeships
Registered apprenticeships are “earn-and-learn” models that have been validated by the U.S. Department of Labor or a State Apprenticeship Agency. There may be federal workforce funding available to support employers and individuals seeking to undergo training to earn a nationally-recognized credential. In the direct care workforce space, registered apprenticeship programming has already been developed for Nursing Assistants and Social and Human Service Assistants, but there may be an opportunity to build programming for other direct care roles.
- As an example, Missouri has multiple nurse assistant registered apprenticeship programs and the Missouri Department of Mental Health has recently developed a Direct Support Professional registered apprenticeship program
Benefits of Registered Apprenticeships to Incumbent Workers and Employers:
- Assistance with training and tuition costs (On-the-Job-Training contracts can reimburse employers up to 75 percent of wage rates paid to participants for up to six months)
- Coverage for supervision and extraordinary training costs (equivalent to 75 percent of the apprentice’s wage rate)
- Provision of additional recruiting, placement, and support services (including transportation, books, supplies, and childcare)
Opportunities for state action:
- To explore whether a registered apprenticeship for direct care roles exists in your state, visit https://www.apprenticeship.gov/apprenticeship-job-finder
- To develop or expand apprenticeship opportunities in the direct care space, consider sharing information about registered apprenticeships and the support provided by state workforce agencies with direct care employers through informational sessions and customized marketing materials.
Work-based Learning
In contrast to registered apprenticeships, work-based learning programming is generally developed at the state level using Workforce Innovation and Opportunity Act (WIOA) funding. These programs may include career and technical education opportunities, and are targeted to a number of audiences, including high school students and adult learners. States or local workforce development boards develop strategies to prioritize the use of work-based learning funding. State approaches vary significantly, but many focus on high-wage, high-skill, and high-demand careers. Although direct care roles are certainly in high demand, they are not generally classified as high-wage or high-skill and therefore may not be prioritized for funding or emphasis by workforce development agencies.
Opportunities for state action:
- Review state strategies for prioritizing occupations for workforce development funding and determine whether direct care roles are included
- This resource by the Education Commission of the States may serve as a helpful guide to identify state strategies for the designation of high-demand occupations which are prioritized for workforce development funding.
- If direct care roles are not currently included and there is interest in prioritizing these roles for workforce development funding, consider alternative strategies or exploring sector or sub-sector specific strategies (such as grant programs for training, tax credits for instructors, or partnering with state Medicaid offices to provide reimbursement increases if direct care workforce development indicators are met).
Career Pathways
Many direct care jobs require skills that may be easily translated through training into higher skills and higher wage health sector opportunities. However, the time and costs associated with additional training make the pursuit of these opportunities challenging. By establishing career pathways that facilitate transitions to higher skills and higher wage jobs in the health sector, it is easier to retain qualified workers in the health sector. Career pathways for direct care roles can be developed alongside apprenticeship and work-based learning opportunities. States can also focus on clearly articulating career pathways for direct care workers, both within direct care roles and into other jobs in the health sector.
Opportunities for state action:
- Leverage state longitudinal data systems or licensing/regulatory data to assess and articulate common career pathways for direct care workers.
- Identify opportunities for the development of stackable and portable credentials for direct care roles, and align steps along the career pathway with paid training opportunities.
- Consider partnering with community colleges for the development of these pathways.
- Create reference documents and resources which clearly articulate direct care career pathways. Share these resources with local American Job Centers and high schools to promote advancement opportunities for direct care workers.
- As an example, Oregon has created and published career lattices for homecare and personal support workers.
DCW Wage Assessment
The fourth consideration in the Issue Brief State Strategies for Sector Growth and Retention of the Direct Care Workforce is “Evaluate Strategies for Addressing Wage Issues.”
Wages for direct care jobs are typically low in comparison with other middle-skills jobs. Nationally, one in eight direct care workers lives in poverty. Competition for workers from the gig economy, paired with lack of professional growth opportunities for direct care workers, can result in high turnover. Reducing attrition remains essential if states are to build a direct care workforce pipeline. While many direct care workers may want to pursue pathways to higher-skilled and higher-credentialed jobs, some may prefer to remain in a position where direct care is their primary responsibility. For these workers, addressing wage issues is a top priority.
As states explore strategies to address direct care worker wage issues, a first step may be to assess the current state of direct care worker wages both in the state and nationally in comparison to those of other occupations. Additionally, states may want to explore what wage strategies were established historically or best practices in other states. Below is a template that states may use to explore these strategies.
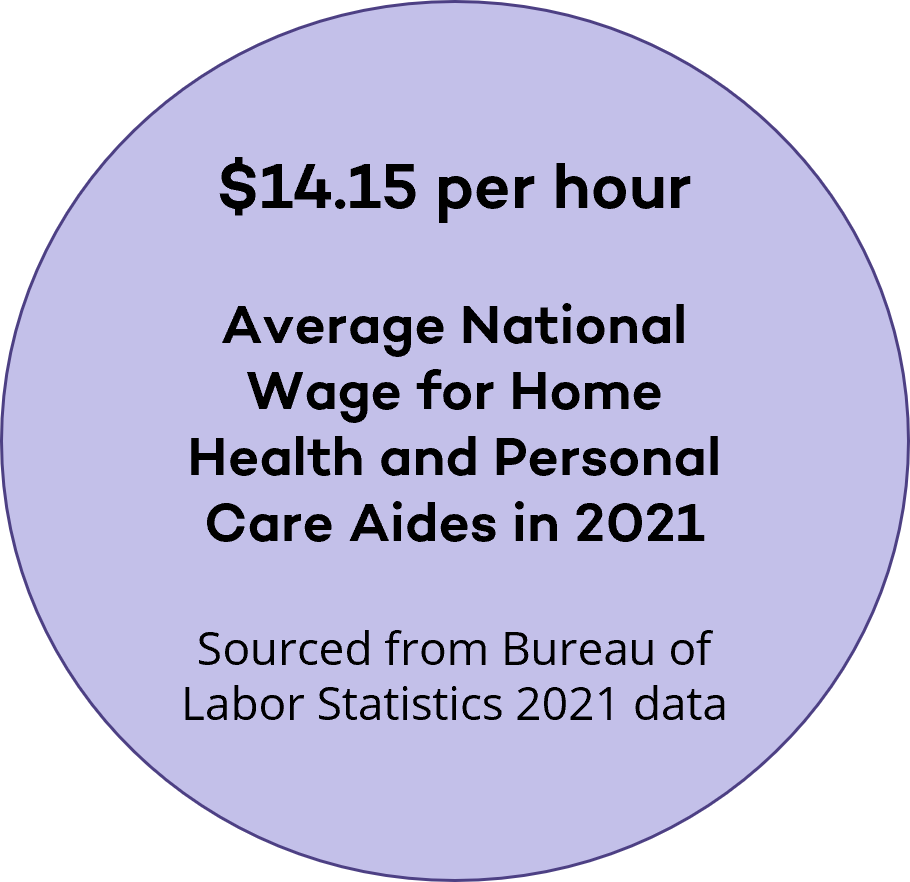
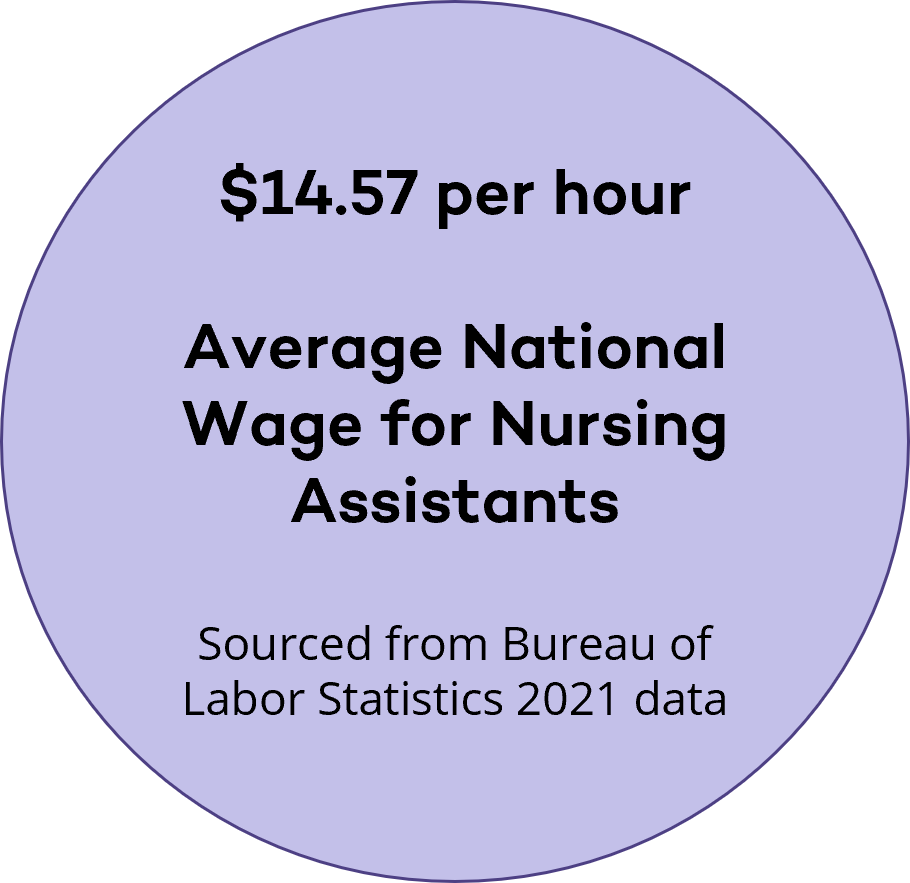
State Direct Care Workforce Wage Assessment
Use the links below to see profession specific hourly wages (1) for your state/territory and compare to living wage (2) estimates.
(1) Hourly wage for:
- Nursing Assistants:
USA | AK | AL | AR | AS | AZ | CA | CO | CT | DE | FL | GA | GU | HI | IA | ID | IL | IN | KS | KY | LA | MA | MD | ME | MI | MN | MO | MP | MS | MT | NE | NC | ND | NH | NJ | NM | NV | NY | OH | OK | OR | PA | PR | RI | SC | SD | TN | TX | UT | VI | VA | VT | WA | WV | WI | WY - Health Aides:
USA | AK | AL | AR | AS | AZ | CA | CO | CT | DE | FL | GA | GU | HI | IA | ID | IL | IN | KS | KY | LA | MA | MD | ME | MI | MN | MO | MP | MS | MT | NE | NC | ND | NH | NJ | NM | NV | NY | OH | OK | OR | PA | PR | RI | SC | SD | TN | TX | UT | VI | VA | VT | WA | WV | WI | WY - Personal Care Aides:
USA | AK | AL | AR | AS | AZ | CA | CO | CT | DE | FL | GA | GU | HI | IA | ID | IL | IN | KS | KY | LA | MA | MD | ME | MI | MN | MO | MP | MS | MT | NE | NC | ND | NH | NJ | NM | NV | NY | OH | OK | OR | PA | PR | RI | SC | SD | TN | TX | UT | VI | VA | VT | WA | WV | WI | WY
(2) State Living Wage Estimates:
AK | AL | AR | AZ | CA | CO | CT | DE | FL | GA | HI | IA | ID | IL | IN | KS | KY | LA | MA | MD | ME | MI | MN | MO | MS | MT | NE | NC | ND | NH | NJ | NM | NV | NY | OH | OK | OR | PA | RI | SC | SD | TN | TX | UT | VA | VT | WA | WV | WI | WY
The Emerging Field Of Behavioral Health Paraprofessionals
State Regulatory Approaches for Peer Specialists, Community Health Workers and Behavioral Health Technicians/Aides
Historically, the workforce supporting behavioral health has generally included health professionals with a master’s degree or higher in education and training. These workers have included counselor-level licensed professionals (such as mental health counselors, clinical social workers, marriage and family therapists, psychiatric advanced practice nurses, etc.) and doctorally trained professionals (such as psychologists and physicians). More recently, states have adopted various approaches toward training and regulating the workforce dedicated to substance use, such as addiction counselors. For these dedicated professionals, states have adopted multiple levels of professional certifications, from peer professionals (people with lived experience with mental health or substance use issues) requiring a high school diploma, to master’s level counselors providing clinical counseling services. In fact, 49 states had a formal credential for peer professionals as of 2023. However, fewer states have formalized training including certifications and licensing for the behavioral health workforce providing support services in a non-peer role or outside of substance use disorder treatment settings.
As such, an emerging topic of interest among states is moving from filling the behavioral health workforce mainly with professionals who have a significant amount of post-secondary education to create opportunities for behavioral health support among professionals with more accessible levels of schooling. This interest is dually inspired by states seeking strategies to address behavioral health workforce shortages and an acknowledgement that current state-credentialed behavioral health roles may be too reliant on those with a master’s degree or other higher trained professionals.
Without additional pathways for employment in behavioral health fields, states may be left with perpetual shortages, prospective workers with training or experience with no current path for meaningful contribution to the behavioral health system, and a long lead time needed to fill roles requiring at minimum many years of post-secondary education and training (four years for bachelor’s degree, two years for master’s degree and two years of experience for full licensure). However, it should be noted that state credentialing approaches for this new subset of the workforce would not be a silver bullet to address behavioral health workforce shortages; there will still be a need for higher level services that can only be provided by certain professionals. States are exploring these credentialing strategies in concert with other strategies to enhance access to behavioral health services, including participation in licensure compacts, education or clinical training expansion, telehealth and other strategies.
As it relates to this “untapped pool” of potential behavioral health workers, little research has been formalized nationally to develop a common terminology for and definition of these workers. However, a recent study by the Bipartisan Policy Center refers to this category of behavioral health workers as “Behavioral Health Support Specialists.”
For the purposes of this brief, the term “behavioral health paraprofessionals” is an umbrella term which will be used to include (but may not be exclusive to) the following roles:
- Peer Specialists (peer support workers)
- Community Health Workers
- Behavioral Health Technicians/Aides
Among these roles, states have implemented different approaches toward regulating and credentialing them. The remainder of this brief provides an overview of state approaches and highlights key examples.
Why Is This Topic of Interest To States?
Without formal roles for behavioral health workers trained with a bachelor’s degree or less, states may have:
- Untapped pools of potential behavioral health workers, with relevant education or experience and no pathway for contribution
- An overworked workforce of masters-level and higher professionals that is relied on to provide supportive services that may not require the depth of specialized training that these providers received
- Long lead times to address their behavioral health shortages if the impact of these investments will not be realized until professional-level behavioral health workers complete training
Peer Specialists (Peer Support Workers)
State regulation for peer support specialists has been a well-developed area of study and assessment. Although the peer specialist role has been around for many decades, the first state regulation for these roles was established in 2001. Since that time, the majority of states have followed suit, with 49 states offering a certification for peer specialists as of 2023.
Peer specialist roles exist in states through two common worker types: substance use and/or mental health recovery. According to an analysis completed by the Peer Recovery Center of Excellence (funded by the Substance Abuse and Mental Health Services Administration (SAMHSA)), state regulation for these roles falls into the following categories:
State Approaches to Peer Specialist Licensing/Certification
| Certification Category | Category Definition | Number of States |
|---|---|---|
| Separate | Separate certifications for Peer Support Specialists with lived experience with substance use or mental health recovery | 13 |
| Integrated | One certification for Peer Support Specialists with lived experience in substance use and/or mental health recovery | 34 |
| Substance Use Only | Certification for Peer Support Specialists with lived experience in substance use recovery | 1 |
| Mental Health Only | Certification for Peer Support Specialist with lived experience in mental health recovery | 1 |
| None | No established Peer Support Specialist certifications. | 1 |
State Role in Regulation
As it relates to state approaches for regulation of these certifications, the state’s role varies widely. The most common approach is for states to provide the certification to qualified individuals directly, but some states defer to (or contract with) third party entities to provide the certification on behalf of the state. For states that provide the certification directly, this function is done most commonly through the state’s executive branch agency dedicated to behavioral health (such as in Arkansas where the Department of Human Services administers the certification), but some states may provide certification through an executive branch entity dedicated to licensing (such as the New Hampshire Office of Professional Licensing and Certification, Board of Licensing for Alcohol and Other Drug Use Professionals).
State Regulatory Standards
Certification requirements also vary substantially across states. Lived experience is the most common requirement among states for both substance use and mental health peer specialists. Education requirements are generally around 40 hours, with an associated written exam. About half of states specify supervised work experience requirements; of those, requirements are generally less than or equal to around 500 hours of experience. Most states do not require a criminal background check. However, of those that do, some states outline which criminal offenses would disqualify an individual from being certified. Additional information about state requirements for peer support certifications can be found in the previously referenced report, Comparative Analysis of State Requirements for Peer Support Specialist Training and Certification in the United States. Additional information about peer support certification models and standards can be found in the SAMHSA report National Model Standards for Peer Support Certification.
A Snapshot of Peer Specialists
- How do states regulate these workers? Most often through state certification/credentialing
- What is required to become one? Lived experience as an individual or as a family member of an individual in substance use recovery or mental health recovery, completion of state training, demonstration of competencies
- What do these workers do? Provide non-clinical supports to others seeking recovery
- What are other titles for these professionals? Peer Recovery Specialist, Peer Specialist, Peer Mentor, Recovery Coach, etc.
Community Health Workers
Community Health Workers (CHWs) are another category of behavioral health support specialists. CHWs are defined as “frontline public health workers that are trusted members of the community they serve.” These individuals engage with communities and community members to facilitate connections with the health care system and address social drivers of health.
Connection between Community Health Workers and Behavioral Health
Over the last decade and a half, the role of CHWs in mental health interventions has been the topic of research as well as exploration by states. Findings suggest that, with the appropriate training, CHWs may be able to support the delivery of mental health interventions, expanding access to care for underserved populations. No standardized or widely accepted mental health training currently exists for CHWs. Given this, states have the opportunity to develop their own approach to train and deploy CHWs to provide behavioral health support. The extent to which CHWs specialize in or serve in behavioral health settings or roles varies by state and by individual CHW. For example, the Michigan Medicaid reimbursement model reimburses CHW services for members under the Behavioral Health Home and Opioid Health Home programs for specialty behavioral health populations.
State Role in Regulation
Several states have developed certification and training standards for CHWs through a variety of approaches. As of 2024, 25 states have a CHW Certification program. Certification is typically voluntary to provide CHW service—in other words, CHW services can be legally provided without the certification. However, in many states, certification is required in order to access Medicaid funding.
A recent state tracker from the National Academy for State Health Policy found that 24 states have supported Medicaid reimbursement for CHW-provided services by amending their state plan through the section 1115 waiver process, through encouraging or requiring managed care organizations to support CHW services, or some combination. As it relates to states’ specific role in the certification of CHWs, states with certification programs usually administer their own credentialling, and this is generally through their health or human services department.
As an example, Arizona defines the CHW role in statute (A.R.S. 36-765(2)) and administrative code (R9-16-802(C)(D)) and defines an optional credentialing pathway through their Medicaid agency (Arizona Health Care Cost Containment System). Other state certification approaches include the use of independent credentialing boards or working with a local CHW professional association to manage credentialing.
State Regulatory Standards
In order to qualify for certification as a CHW, states generally require state-approved or administered training, which generally align with CHW competencies outlined in the CHW Core Consensus Project. However, some states also require demonstration of hours of experience or provide experience as an alternate pathway to certification.
A Snapshot of Community Health Workers
- How do states regulate these workers? Either no regulation or through voluntary certification standards to access Medicaid reimbursement
- What is required to become one? For those seeking voluntary state certification, state-approved or administered training
- What do these workers do? Serve as an intermediary between clients/patients and health or social services in the community
- What are other titles for these professionals? Community health worker is the most common title
Behavioral Health Technicians/Aides
The final category of behavioral health support specialists is behavioral health technicians/aides. This role of paraprofessionals in the behavioral health space is an emerging area of interest for states. These roles are commonly seen as extenders of behavioral health services for activities that do not require professionals trained with a master’s degree or higher.
Behavioral health technicians/aides are distinct from peer specialists and community health workers in that they generally do not require lived experience, but instead focus on state-approved or state-provided training. However, in some cases, experience (lived or other) does serve as a qualifying pathway. Additionally, behavioral health aide/technician functions and duties vary widely across state implementation models.
Before discussing state implementation approaches for these roles, it is important to note that this is an emerging field, and no single term has been designated to refer to these roles. For the purposes of this brief, the term “behavioral health technician/aide (technician/aide)” will be used. Other terms that have been put forth by states and in the research include “behavioral health support specialists,” “behavioral health aide,” “behavioral health paraprofessional” or “psychiatric technician.”
A Snapshot of Behavioral Health Technicians/Aides
- How do states regulate these workers? State defined training is commonly required; some implementation models result in a state certification/license to provide the related services or in certain settings
- What is required to become one? Most models include state defined training or accepted education levels; in many cases, these roles must function under the supervision of a higher-level professional
- What do these workers do? Job functions vary widely across states but generally provide supportive services to provide screenings, implement treatment plans and patient education
- What are other titles for these professionals? Behavioral health support specialists, Behavioral Health Aide, Behavioral Health and/or Psychiatric Technician, Wellness Coach, etc.
State Role in Regulation and State Standards
State approaches to regulation for technician/aide roles vary widely. For states with formalized roles, guidelines are developed through statute, rules, Medicaid modules, or other state programming to define these roles and associated entry criteria. Below are categories of state approaches offered for consideration, with examples of states that have implemented that strategy:
Defined technician/aide role in state code or rules
One approach states have taken is to define the technician/aide role within state statute or rules. To achieve this, the definition must have gone through either the legislative or executive branch rule-making process. For states that have followed this approach, the extent to which the role is defined varies; some states define the role and associated services/scope of practice without having formal training requirements, while others may define the role and outline training and/or certification requirements. Below are examples of states that have defined the role within statute or rules:
Statutorily defined role with state-outlined training requirements, both with and without formal certification.
- Minnesota Mental Health Behavioral Aides: Minnesota has developed a Mental Health Behavioral Aide (MBHA) occupation modeled after Alaska’s Behavioral Health Aide model, see below. MBHAs are outlined within Minnesota statute (45I.04.16). This MBHA role requires approximately 30 hours of pre-service state training. MBHAs support children with mental illness by helping them develop skills under their individual behavioral plan. A Level I MBHA requires a high school diploma and two years of experience (no formal certification), whereas a Level II MBHA requires at least an associate degree and formal certification (administered after receiving state training provided through a university partnership).
- Minnesota Mental Health Practitioners: Minnesota has “Mental Health Practitioner” (MHP) roles that are eligible to provide certain treatment services to adult clients (education, rehabilitative services, functional assessments, level of care assessments, treatment planning, and crisis assessments/interventions) and child clients (skill-building, treatment plans). This role is statutorily defined (245I.04.4) to include a variety of education/experience qualification paths (including pathways for individuals with lived experience, current college students, those not fluent in English, those with at least 30 hours of college experience and masters-trained professionals). MHPs work under the supervision of a mental health professional. There is no formal state certification associated with this role.
- Minnesota Mental Health Rehabilitation Workers: Minnesota also has an adult population-focused role, called “mental health rehabilitation workers,” which provides basic living and social skills under rehabilitative mental health services. Like the MHP role, there are various pathways to qualify to serve in this role, including formal academic training (associate degree), qualifying experience (>2,000 hours) or lived experience. There is no formal state certification associated with this role.
- Utah Behavioral Health Technicians and Behavioral Health Coaches: Utah recently developed two state-certified behavioral health aide/technician-type roles through statute: “behavioral health technician” and “behavioral health coach.” The behavioral health technician role requires completion of a one-year certificate program or an associate degree in a qualifying field. The behavioral health coach role provides two pathways to certification: 1) a higher education pathway through completion of a bachelor’s degree in a qualifying field and a letter of recommendation to verify competency; or 2) a “stackable” credential and experience pathway which can be achieved through completion of an associate’s degree or higher in a relevant field, two years of experience as a technician or other relevant role (such as peer support specialist, case manager, etc.), and a letter of recommendation to verify competency.
- Wyoming Certified Mental Health Workers: Wyoming utilizes a “certified mental health worker” (CMHW) role, which is defined through statute with entry requirements defined in rules and regulations. CMHWs are individuals with a bachelor’s degree or higher in a human behavioral discipline who have met relevant coursework requirements, have experience under direct and indirect supervision (500 hours total) and who have successfully passed a state-defined examination. CMHWs receive certification through the Mental Health Professions Licensing Board and can provide assessment, treatment, and prevention-related services under the supervision of a designated qualified clinical supervisor (fully licensed behavioral health professional or advanced practitioner).
Role defined through regulation, with associated training requirements but no certification.
- Arizona Behavioral Health Paraprofessionals: Arizona has implemented a title for the role of “Behavioral Health Paraprofessionals” which are non-Behavioral Health Counselor staff providing behavioral health services in a facility-based setting, under the supervision of a behavioral health professional. The role is defined in Arizona regulations (A.A.C. R9-10-101(34)) as “an individual who is not a behavioral health professional who provides behavioral health services at or for a health care institution according to the health care institution’s policies and procedures that: (a) If the behavioral health services were provided in a setting other than a licensed health care institution, the individual would be required to be licensed as a behavioral professional under A.R.S. Title 32, Chapter 33; and (b) Are provided under supervision by a behavioral health professional.” The Arizona Department of Health Services (ADHS) has also provided guidance for employers related to the Behavioral Health Paraprofessional role. The Arizona Health Care Cost Containment System rearticulates the ADHS definition of the paraprofessional role and specifies education requirements in guidance for employers/providers. Professional requirements for this role include at least a high school diploma and having the knowledge necessary to provide the service (as verified by a clinical director).
- Arizona Behavioral Health Technicians: In addition to Arizona’s Behavioral Health Paraprofessionals role, the role of Behavioral Health Technician is also defined within Arizona regulations (A.A.C. R9-10-101(39)). The Technician role has associated clinical oversight requirements. Compared to the Paraprofessional role, the Technicians play a more substantial role in behavioral health service delivery, including conducting assessments, counseling, and implementing treatment plans (with specified clinical oversight requirements met). The Arizona State Plan specifies the level of education/degree required to serve as a Technician; this includes a wide range of experience/education, from an individual with a high school diploma and at least four years of related experience, to an individual with an associate, bachelor’s or master’s degree in a related field. While not defined in statute, the Behavioral Health Technician and Behavioral Health Paraprofessional roles are exempted from licensure per statute.
- Oregon Qualified Mental Health Associates: Oregon has various pathways to become a paraprofessional through rule-defined Qualified Mental Health Associate (QMHA) roles (OAR 309-019-0125(9)(a)(b)). Additional guidance is provided by the Mental Health and Addiction Certification Board of Oregon. There are both degree and non-degree (experience) pathways to certification. Certification is required to serve in these roles within state-certified mental health programs. QMHAs are eligible to provide a number of behavioral health services in the state fee schedule under mental health outpatient services, including case management, screenings, activity therapy and patient education.
Defined technician/aide role in state guidance or Medicaid modules
As an alternative to outlining this role in state code or rules, many states have defined a role within an executive branch agency or division’s guidance. For example, some states have included information on their website which specifies the role, or the role has been defined within Medicaid provider modules or service delivery guidelines. State approaches to training and certification for these roles also vary. Below are examples of roles outlined in non-statute or rule mechanisms:
- Executive branch agency-defined role with state training without formal certification. Georgia uses “paraprofessionals” (individuals with or without a bachelor’s degree) to provide a variety of services under their Community Behavioral Health Providers module. Paraprofessionals are individuals with (Level 4 staff) or without (considered Level 5 staff) a bachelor’s degree who have completed a state-required training module.
- Executive branch agency-defined state training and associated formal certification. Alaska developed a “Behavioral Health Aide/Practitioner” (BHA/P) role to provide behavioral health services to community members and clients of a Tribal Health Organization within the Alaska Tribal Health System. There are various levels of BHA/P roles, each with varying expectations for training/education and experience. Each level results in a state certification which must be renewed every two years. BHA/Ps are generally members of the community they serve, meaning this role could be categorized as either a community health worker or behavioral health technician/aide. BHA/Ps serve under masters-level behavioral health clinicians. BHA/Ps can provide a number of services under the Indian Health Service, but also serve as Qualified Addiction Professionals under Alaska’s Medicaid substance use disorder plan. Of note, Alaska has developed a number of hiring and onboarding resources to support recruitment of prospective BHAs, including recent high school graduates.
- Executive branch agency-defined state training and associated formal certification. Maine has a state training and certification for a “Mental Health and Rehabilitation Technician (MHRT)” through the Department of Health and Human Services. MHRTs work with adults with serious mental illness and are specialized into one of three categories: Community (MHRT/C), Residential (MHRT/I) and Crisis Service Provider (MHRT/CSP). MHRTs are categorized in state Medicaid programming as “other qualified mental health professionals.” There are various pathways to qualify for state MHRT Certification, including traditional academic training (bachelor’s degree), completing a qualifying program at state-approved program, or completing free training online with at least 12 months of experience.
State Approaches to Behavioral Health Technician/Aide Licensing/Certification (A Sample)
| | Formalization of Role | State-defined Training Requirements | Scope of Practice/Services | State Certification |
|---|---|---|---|---|
| Alaska Behavioral Health Aide | Alaska Tribal Health System guidance, State plan | Yes; delivered through non-profit | Remote community-based settings under employment by Indian Health Service or state Medicaid | Yes |
| Arizona Behavioral Health Paraprofessionals | Executive branch rules | Yes; high school diploma or greater, skills/knowledge verified by the clinical director | In health care institutions; under supervision by a behavioral health professional | No |
| Arizona Behavioral Health Technician | Executive branch rules | Yes; high school diploma + 4 years of experience or greater; includes various educational backgrounds | In health care institutions; under clinical oversight by a behavioral health professional | No |
| Georgia Paraprofessionals | Medicaid provider manual | Yes; delivered through learning management system | Community-based settings; services vary based on level of paraprofessional | No |
| Maine Mental Health and Rehabilitation Technician | State guidelines | Yes; various pathways to role including state-developed/administered online training | Community-support services to adults with serious mental illness | Yes |
| Minnesota Mental Health Behavioral Aide (MHBA) Level I | Statute | Yes; high school diploma and 2 years of experience | Psychosocial skills with child; under treatment supervision of mental health professional | No |
| Minnesota Mental Health Behavioral Aide Level II | Statute | Yes; associate degree or higher plus 30-hour training | Psychosocial skills with child; under treatment supervision of mental health professional | Yes |
| Minnesota Mental Health Practitioner | Statute | Yes; various pathways to role | Variety of services (including direction to MHBAs and MHRWs); under treatment supervision of mental health professional | No |
| Minnesota Mental Health Rehabilitation Worker (MHRW) | Statute | Yes; various pathways to role | Rehabilitative mental health services, under treatment supervision of mental health professional | No |
| Oregon Registered Mental Health Associate (Qualified Mental Health Associate-Registered, QMHA-R) | Statute, Medicaid guidelines | Yes; bachelor’s degree in relevant field or combination of at least three years of relevant education and experience | Application of communication, mental health assessments, treatment and service terminology competencies; skills development; identification, implementation and coordination of services and supports from treatment plan | Yes |
| Oregon Basic Mental Health Associate Certification (QMHA-I) | Statute, Medicaid guidelines | QMHA-R plus 1,000 supervised hours in relevant competencies and associated Level I exam; biannual recertification and 40 hours continuing education | Yes | |
| Oregon Advanced Mental Health Associate Certification (QMHA-II) | Statute, Medicaid guidelines | QMHA-I plus minimum of 4,000 supervised hours in relevant competencies and associated Level II exam; biannual recertification and 40 hours continuing education | Yes | |
| Utah Behavioral Health Technician | Statute | One-year academic certificate or associate degree or higher in relevant field | Under supervision of mental health therapist: supporting administrative and care coordination; non-clinical assessments, monitoring and care planning; supporting intervention and treatment | Yes |
| Utah Behavioral Health Coach | Statute | Higher education pathway: bachelor’s degree or higher in relevant field; letter of recommendation Stackable credentials and experience pathway: associate degree or higher in relevant field, letter of recommendation, two years full-time work experience in relevant role | Administrative and care coordination; patient assessment/monitoring; intervention and treatment (under supervision of mental health therapist); co-facilitating group therapy with mental health therapist | Yes |
| Wyoming Certified Mental Health Worker | Statute, Rules | Yes; bachelor’s degree in relevant field, 500 hours of experience, examination | Assessment, treatment and prevention-related services under supervision | Yes |
Considerations
As states seek to address behavioral health workforce challenges, the development of formal roles is a strategy to create a meaningful pathway for mental health workers who do not qualify as therapists, social workers, counselors, psychologists or other traditional roles. For states that may be interested in exploring the establishment of these roles through regulation, below are key considerations:
- Financial Sustainability. As described above, the establishment of many of these formal state credentialing initiatives is done by or in concert with state Medicaid programming. Coordination with a payer source supports the financial viability of these roles and the contributions these workers make to behavioral health service delivery.
- Stackable Credentials. Among the states with paraprofessional roles, many have developed tiers which align with education or experience requirements and additional levels of services that can be provided by higher tier roles. This framework provides a pathway for growth and development among paraprofessionals and could be built out to create a cohesive ladder to master’s level and other higher-level roles.
- Reciprocity. State approaches to formalization of these roles, particularly with the paraprofessional roles, vary widely. Given the lack of standardization among states, states may consider how to support interstate mobility of these professionals. Pathways for reciprocity can be acknowledged and formalized alongside in-state qualification pathways. Specifically for peer specialist roles and in acknowledgement of a greater likelihood that these individuals may have criminal histories, it may be important to consider enhanced transparency of disqualifying crimes and pathways for remediation, both for reciprocity and career pathway buildouts for these roles.
- Coordination with Other Strategies. In many state models, the services provided by behavioral health support specialists (especially paraprofessionals) require supervision by other behavioral health roles, typically licensed professionals. Specific supervision provisions vary, but generally some amount of a licensed professionals’ time is required. Given the ubiquitous nature of workforce shortages in behavioral health, it is important for states to consider the broader impact of these strategies on the overall workforce and ensure coordination across approaches to support the behavioral health workforce broadly.
This publication was developed by Courtney Medlock and Dr. Hannah Maxey of Veritas Health Solutions on behalf of the National Governors Association Center for Best Practices (the NGA Center). The NGA Center would like to thank the Health Resources and Services Administration in the U.S. Department of Health and Human Services for their generous support in the development of this publication under National Forum Cooperative Agreement No. U98OA09028. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of HRSA or the U.S. Department of Health and Human Services.
Additional Resources
- ADvancing States
- PHI
- Millbank and Center for Health Strategies: Direct Care Workforce Policy and Action Guide
- Stay tuned for more information on the forthcoming ACL National Center to Strengthen the Direct Care Workforce