This report outlines considerations and examples of strategies for leveraging PCPs to increase COVID-19 vaccine uptake.
(Download)
As supply of the COVID-19 vaccine has eclipsed demand in many areas across the country, states are shifting strategies to increase accessibility and engage communities with low vaccine uptake. With over 80 percent of adults receiving care through a regular medical home, primary care providers (PCPs) are critical to reaching the nine percent of surveyed adults who have not received the vaccine but expressed keen interest getting it, as well as the 15 percent with additional questions indicating they would like to “wait and see”. In a recent Kaiser Family Foundation (KFF) survey, half of individuals in the “wait and see” group said they would be more likely to get the vaccine if it were offered during a routine medical visit – indicating the critical role PCPs play in this effort. Moreover, surveys show health care providers as the most trusted source of COVID-19 vaccine information for patients, and pediatricians will play an ever-increasing role in vaccinating 12 – 15 year-olds in the near-term and younger children in the longer-term.
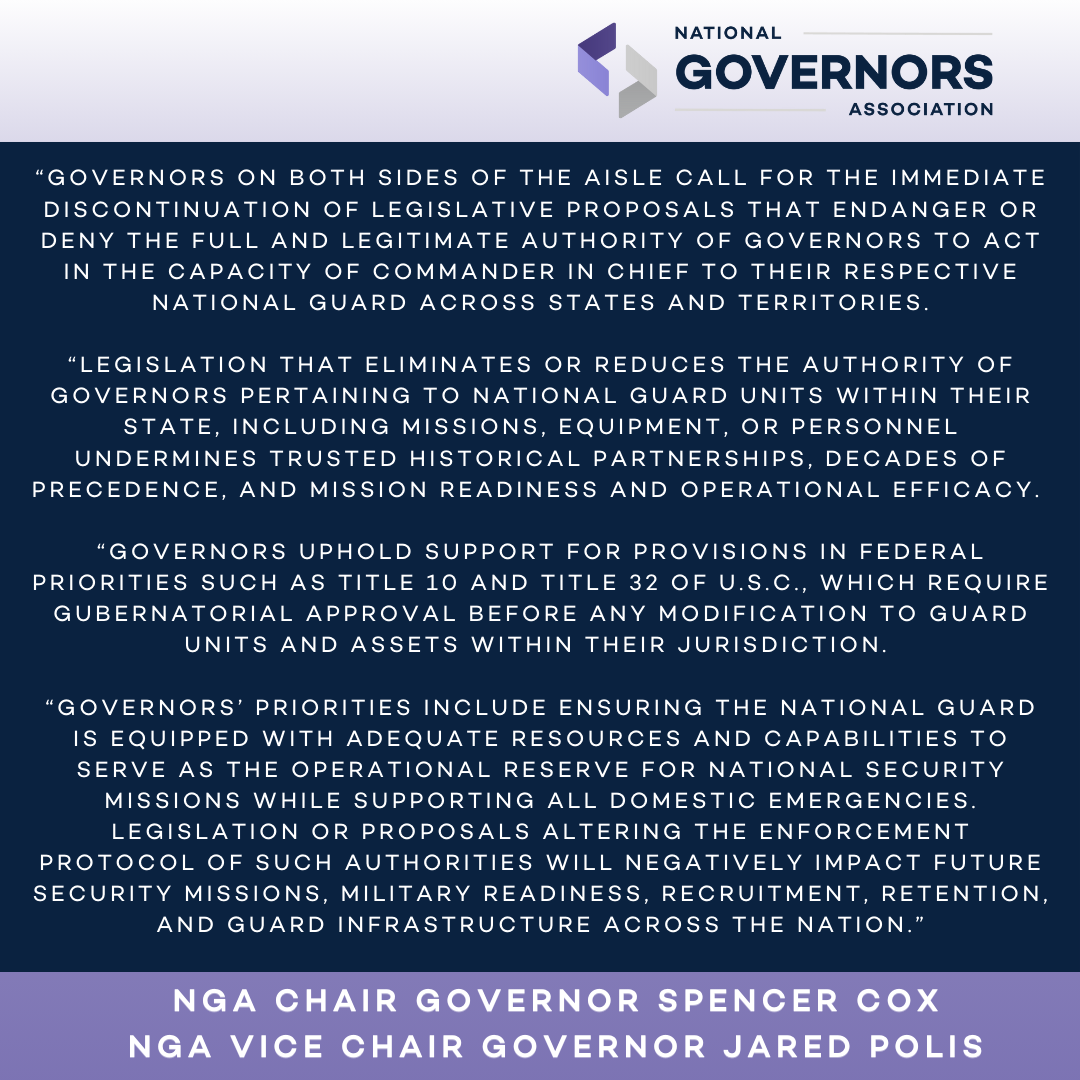
To reach those not yet vaccinated for COVID-19, states are shifting away from high-throughput sites and towards convenient community settings such as primary care offices, health clinics, pharmacies, schools, workplaces and mobile or pop-up sites. A key strategy in the next phase of pandemic response is to engage PCPs as trusted resources for vaccinations. The National Governors Association (NGA) and Duke-Margolis Center for Health Policy (Duke-Margolis) interviewed a sample of states and conducted targeted research to identify promising practices for Governors to engage and leverage PCPs as COVID-19 vaccinators. This report summarizes these findings, providing Governors and state officials with considerations and examples of strategies for leveraging PCPs to increase COVID-19 vaccine uptake.
Considerations for Governors
Based on interviews of key stakeholders and additional research, NGA and Duke-Margolis identified five categories of strategies for Governors and state officials to use in engaging and supporting PCPs (including pediatricians) as vaccinators. These strategies include:
- Engage, enroll and provide technical support for primary care providers
- Address logistical and distribution challenges to support vaccine administration in primary care settings
- Offer clear guidance prioritizing “shots in arms” over concerns about speed or waste
- Incentivize provider participation through reimbursement policies and other financial support
- Provide resources and support for communicating with the public and engaging communities
Engage, Enroll and Provide Technical Support for Primary Care Providers
During the initial phases of vaccine distribution states prioritized high-throughput sites such as large health systems, retail pharmacies and mass vaccination clinics. As states shift to community-based approaches, identifying and enrolling PCPs will require partnerships with provider associations, low-barrier enrollment processes and ongoing technical assistance. PCPs may face a variety of challenges enrolling in state immunization information systems (IISs), complying with storage requirements, meeting COVID-19 vaccine Emergency Use Authorization (EUA) conditions (e.g., raising awareness of risks to specific populations) and/or integrating vaccinations into routine clinical care.
Governors and state officials may consider the following to support provider enrollment and engagement:
- Conduct outreach to enroll eligible providers and facilitate onboarding with the state’s IIS.
- Partner with state-affiliated primary care associations to reach eligible vaccinators and support enrollment.
- Provide training, guidance and support to build provider capacity.
- Issue consistent guidance and communication on training, storage, wastage and sharing best practices among and between states.
- Offer multiple avenues of feedback and Q&A, such as town halls and surveys.
Examples of state strategies for engaging, enrolling and providing technical support for PCPs include:
- The Maryland Department of Health has conducted 98 webinars since the beginning of the COVID-19 pandemic, with a recent meeting educating the primary care workforce on proper administration, storage and handling of COVID-19 vaccines.
- Michigan is deploying six field representatives to provide local health departments with technical assistance and support for PCPs as they onboard as COVID-19 vaccinators. Additionally, the state developed a checklist and resource toolkit for providers as they prepare their offices to administer COVID-19 vaccines. Also, the state releases a weekly newsletter called “The Provider Brief” and holds a bi-weekly webinar called “Noontime Knowledge” to update and educate COVID-19 vaccination providers. A recent webinar included an update on vaccine storage and handling guidance in primary care settings.
- North Carolina is collaborating with its provider associations to recruit practices, provide educational webinars and offer hands-on enrollment workshops. The state has engaged health systems and payers to conduct outreach and recruit providers, especially in priority areas with low vaccination rates and high social vulnerability. The state has a dedicated team to walk practices through the enrollment process and provide technical assistance through nurse consultants and case managers or its suite of guidance documents.
- Rhode Island is taking a phased approach to onboard PCPs, beginning with large family medicine and pediatric practices. The Rhode Island Department of Health is working through a list of all practices enrolled in the State-Supplied Vaccine Program and contacting providers directly to determine interest and facilitate onboarding.
Address Logistical and Distribution Challenges to Support Vaccine Administration in Primary Care Settings
Major barriers for administering COVID-19 vaccines in primary care settings are the large shipment sizes and storage requirements that may be more difficult to meet in areas with low vaccine uptake and limited resources.[1] Although Pfizer-BioNTech is working to supply states with smaller shipping packages that can facilitate smaller minimum orders for providers, current Pfizer vaccine shipments contain 195 vials holding roughly 1,170 doses. This is especially challenging to pediatric practices as populations aged 12-18 are only authorized to receive the Pfizer vaccine. To respond to these logistical challenges, states have developed approaches to help distribute smaller quantities to PCPs within independent practices, community health centers and practices affiliated with larger health systems.
Governors and state officials may consider the following to address distribution and logistical challenges:
- Encourage cross-system and jurisdictional collaboration to facilitate appropriate stewardship of doses to minimize waste.
- Facilitate community-based partnerships to store vaccines and allow providers to obtain smaller quantities.
- Utilize the national guard to break down doses at central or regional hubs to distribute smaller quantities of the vaccine, allowing practices to receive appropriate quantities and redistribute doses on the ground.
- Work with health systems with affiliated primary care and pediatric offices to serve as hubs and distribute smaller quantities to their affiliated outpatient clinics and pediatric offices.
Examples of state strategies for addressing logistical and distributional challenges include:
- Alaska is developing processes to pick up unused doses from PCP clinics in urban areas and deliver them to mass vaccination sites when there is still time to use them.
- Louisiana developed a management and relocation protocol, with processes to identify PCPs to receive and administer vaccines that are near expiration before they expire.
- In Kansas, all PCPs enrolled as COVID-19 vaccine providers can order directly from the Kansas Department of Health and Environment, even those not previously receiving doses. Moving to an order-based allocation model allows PCPs to manage their vaccine inventory in a way that is responsive to their patients’ needs.
- Michigan strategically placed nine regional freezers for additional Pfizer vaccine storage that will be utilized for adolescent vaccinations and assist with redistribution.
- North Carolina allows providers to request the necessary number of doses on a flexible timeline and encourages self-initiated matchmaking through a weekly list of providers with unused vaccines. In addition to deploying the national guard to deliver smaller quantities, the state is also setting up regional repositories and distribution hubs at health systems with adequate storage with locations selected by local health departments.
- Pennsylvania is actively working with health systems to distribute smaller quantities to affiliated outpatient and pediatric clinics. The state plans to match unaffiliated providers with those able to redistribute smaller quantities of the vaccine. Also, the state requested large health systems partner with PCPs to host vaccination clinics for their patients, rather than administering it themselves. Additionally, Pennsylvania is developing a hub and spoke model to ship Pfizer vaccines to providers with cold storage capability, then redistribute to smaller practices within their service area as needed.
- Virginia made it possible for providers to order smaller quantities of vaccine by using the health department’s central pharmacy, as well as local health departments, to receive, repackage and redistribute vaccine.
- The Washington State Department of Health created a Vaccine Marketplace for providers enrolled with the state’s IIS. Providers with extra doses can share information through the program for providers to request.
Offer Clear Guidance on Prioritizing “Shots in Arms” over Speed or Waste
Initially, many states promoted efficiency in administration by requiring that providers use doses within 7 days of receipt and discouraging providers from wasting doses. These requirements often hindered participation of PCPs, who may not see patients at a sufficient volume to administer all doses received within a 7-day timeframe. As vaccine supply now exceeds demand, many states removed 7-day requirements and changed messaging to emphasize a “no missed opportunity” approach for vaccination. On May 18, the Centers for Disease Control and Prevention (CDC) issued guidance advising providers to vaccinate every eligible person who presents at a vaccination site, even if it means puncturing a multidose vial without having enough people available to receive each dose. While every effort should be made to minimize waste, state leaders have communicated with providers—both through formal guidance and ongoing contact—that the top priority is vaccine accessibility.
Governors and state officials may consider the following to address PCP concerns that they may be penalized for administering vaccines too slowly or wasting doses:
- Remove timeframe requirements that all received doses must be administered within 7 or 14 days.
- Issue wastage and redistribution guidance, emphasizing the importance of available onsite vaccinations.
Examples of state and local strategies for offering clear guidance on priorities include:
- North Carolina removed the 7-day requirement, allowing providers to request doses on an as-needed basis without fear of being penalized for not administering their total allotment, and widely promotes CDC guidance on wastage and avoiding missed opportunities for vaccination.
- Vermont issued guidance advising PCPs to offer vaccines to eligible populations at every encounter and keep a standby list in case there is an open vial with unused doses at the end of the day.
- Virginia’s communication to providers has focused on reassurance about possessing multiple weeks of vaccines and not hesitating to open a multidose vial if there is a patient ready to be vaccinated.
- The Washington Department of Health offers flexibility to certain providers with throughput and usage, including those serving smaller communities, supporting equity efforts and/or reaching special populations, such as hospitals that transfer patients to long-term care facilities.
Incentivize Provider Participation through Reimbursement Policies and other Support
Administration of COVID-19 vaccines can involve additional costs to PCPs compared to other vaccines due to storage and handling constraints, personal protective equipment and reporting requirements. To incentivize providers and offset these costs, the Centers of Medicare and Medicaid Services (CMS) increased the Medicare provider administration rate from $28.39 for a single dose or, for the two-dose series, $16.94 for the first and $28.39 for the second to $40 per vaccine dose; many states adopted this rate in their Medicaid programs. States may also opt to provide financial support to primary care efforts using federal funding for vaccination activities or consider potential options for incentive payments within the Medicaid program.
Examples of sate strategies for boosting participation through financial support include:
- Massachusetts initially set administrative reimbursement rates for MassHealth providers above the Medicare rate while requiring commercial insurers to meet or exceed the CMS rate to ensure that payment would not be a barrier to provider participation in vaccination efforts. The rates were adjusted to align with the Medicare rate after the rate was revised.
- North Carolina increased their Medicaid administration fee to $40 per dose and is exploring fiscal incentives for providers using state dollars while encouraging payers to consider financial and non-financial incentives.
- The West Virginia Primary Care Association received $475,242 through the American Rescue Plan to provide training and technical assistance to health centers as they administer the COVID-19 vaccine. Additionally, the state partnered with an academic institution to develop and offer continuing medical education (CME) credits for providers to learn how to educate patients and build vaccine confidence, an additional incentive to recruit PCPs for COVID-19 vaccination efforts.
Address Barriers for Communities with High Social Vulnerability
In areas with limited vaccine providers, states can work with primary care associations to identify and encourage potential vaccinators, as well as support providers and community health clinics serving under-vaccinated communities. Additionally, individuals with a high degree of social vulnerability may be less likely to have a regular PCP, highlighting the importance of leveraging mobile strategies and matching providers with community-led efforts to supplement challenges in provider access.
Examples of state strategies for addressing barriers in areas with high social vulnerability include:
- Maryland allocates doses to PCPs that serve predominantly Black or Hispanic individuals or to providers serving a large patient base where they can identify and target disproportionately affected patients.
- North Carolina created a public tool mapping social vulnerability, the location of vaccine providers and vaccination rates by census tract which facilitated an increase in vaccinations by 50 percent in 89 of 90 identified communities. The state uses these data to prioritize enrollment of providers in under-resourced communities and identify “Pfizer deserts.” North Carolina shared the prioritized areas and associated unenrolled practices with professional medical societies and health systems to get recruitment assistance for these PCPs. Moreover, the state builds transparency and shared accountability by issuing equity and self-service reports to all vaccine providers. Moreover, the University of North Carolina Center for Health Promotion and Disease Prevention offers coaching, data and community partnership to 18 primary care clinics in areas where vaccination rates are lowest to increase vaccine uptake.
- Washington announced a transition from mass vaccination sites to mobile units staffed with PCPs to take vaccines directly into communities and serve those disproportionately impacted by COVID-19, including counties where data has shown higher gaps in vaccine administration based on race/ethnicity, communities with recent outbreaks or increased cases and hospitalizations, and those with lower vaccination rates.
Provide Resources and Support for Communicating with Patients and Engaging Communities
Building vaccine confidence and ensuring easy access requires a concerted, collaborative effort among providers, public health officials, community leaders and policymakers. As such, increasing vaccine confidence can be addressed through both individual-level efforts, such as patient interactions with their PCP and community-wide media campaigns that leverage PCPs as trusted messengers. PCPs can target their patient populations and address individual concerns while public health leaders can amplify evidence-based, clear messaging encouraging individuals to contact their provider about COVID-19 vaccines.
Governors and state officials may consider the following to support outreach and communication to unvaccinated populations:
- Assist PCPs hosting community clinics or offering flexible hours with resources, staffing and financial support.
- Coordinate educational campaigns that empower unvaccinated individuals to talk with their PCPs to build vaccine confidence.
- Deploy mobile vans staffed with PCPs to provide evidence-based information to unvaccinated individuals in rural and frontier areas.
- Develop purpose-built resources for PCPs, such as provider manuals and how-to guides.
- Support providers with outreach and messaging for unvaccinated patient populations.
- Utilize and communicate with local leaders and grassroots organizations to empower them with toolkits, talking points, posters and social media assets to encourage individuals to get vaccinated.
Examples of state strategies for supporting PCP communication to unvaccinated populations include:
- The Kansas Department of Health and Environment collects data and analytics on specific barriers to vaccine uptake, which PCPs can use to inform conversations with their patients. The state is also developing a manual for PCPs on creating and sending patients mass emails and text messages encouraging vaccination.
- Louisiana Governor John Bel Edwards joined state and national health officials and the American Academy of Pediatrics to urge young people, their parents and all adults to get the COVID-19 vaccine as soon as it is available.
- Maryland Governor Larry Hogan visited clinics providing COVID-19 vaccines to amplify best practices and encourage PCPs to become vaccinators. Additionally, providers enrolled in the state Department of Health’s Maryland Primary Care Program can view their patient list through the state’s health information exchange to determine an individual’s vaccination status. Based on this list, providers can directly order vaccines through the state’s IIS and conduct targeted outreach.
- Michigan’s State Extension Office is working with community leaders and farmers to vaccinate rural communities using PCPs to staff mobile vaccination clinics and serve as a trusted source to answer any questions related to the vaccine.
- North Carolina created a comprehensive toolkit of patient materials and templates for patient outreach, including a discussion guide and templates for robocalls, patient letters and patient emails. The state is partnering with state medical societies to disseminate these resources.
- Pennsylvania hosts town halls with physicians and public health officials to answer questions around safety and efficacy as well as address concern about vaccine confidence. A recent series focused on parents and caregivers of adolescents to encourage this population to seek information from their PCP.
Conclusion
As states shift to community-level grassroots administration to increase access and uptake of COVID-19 vaccines, state PCP networks will be critical to reach unvaccinated individuals. Additional action will be necessary to 1) identify areas with high social vulnerability, low coverage rates and lack of provider access and 2) implement strategies to address this gap in access. PCPs have an immediate role to play to improve vaccine uptake and will be integral in sustaining these efforts should boosters or seasonal administration of COVID-19 vaccines become necessary. Looking ahead, identifying opportunities to integrate PCPs into the evolving COVID-19 vaccine distribution infrastructure will be paramount to ensure community and population-wide protection.
Authors
This publication was developed by Kirk Williamson, Katie Greene and Hemi Tewarson* at the Duke-Margolis Center for Health Policy, in partnership with Michelle LeBlanc and Brittney Roy at the National Governors Association Center for Best Practices.
*Hemi Tewarson contributed to the development of this report during her tenure at the Duke-Margolis Center for Health Policy.
Acknowledgements
The NGA Center and Duke-Margolis would like to acknowledge and thank state officials who granted informational interviews, reviewed drafts and provided content for this publication. The NGA Center and Duke-Margolis also thank the Robert Wood Johnson Foundation for their generous support for work on COVID-19, including this publication.
Recommended citation format
Williamson, K., Greene, K., LeBlanc, M., Roy, B., & Tewarson, H. (2021 June). State Strategies for Engaging and Leveraging Primary Care Providers as COVID-19 Vaccinators. Washington, DC: National Governors Association Center for Best Practices and Duke-Margolis Center for Health Policy.
[1] On May 20, 2021, the U.S. Food and Drug Administration (FDA) authorized the storage of undiluted, thawed Pfizer-BioNTech COVID-19 vaccine vials in a refrigerator at 2°C to 8°C (35°F to 46°F) for up to 1 month. Previously, thawed, undiluted vaccine vials could be stored in the refrigerator for up to 5 days.